Medical education and research: India
(→Capitation fees gone; private colleges’ fees zoom up/ 2016) |
(→Fees) |
||
| Line 643: | Line 643: | ||
(Put together by TOI's network of health reporters across India) | (Put together by TOI's network of health reporters across India) | ||
| + | |||
| + | ===2021=== | ||
| + | [https://timesofindia.indiatimes.com/india/quota-for-the-rich-28-of-mbbs-seats-cost-over-rs-10-lakh-per-year-in-tuition-fees/articleshow/81371223.cms Rema Nagarajan, March 7, 2021: ''The Times of India''] | ||
| + | |||
| + | [[File: States where tuition fee is over Rs 10 lakh per year, 2021.jpg|States where tuition fee is over Rs 10 lakh per year, 2021 <br/> From: [https://timesofindia.indiatimes.com/india/quota-for-the-rich-28-of-mbbs-seats-cost-over-rs-10-lakh-per-year-in-tuition-fees/articleshow/81371223.cms Rema Nagarajan, March 7, 2021: ''The Times of India'']|frame|500px]] | ||
| + | |||
| + | ''' Quota for the rich? 28% of MBBS seats cost over Rs 10 lakh per year in tuition fees ''' | ||
| + | |||
| + | About 28% of MBBS seats in India cost over Rs 10 lakh per annum in just tuition fees. The high fees effectively makes these seats a quota for the rich, one that is larger than those for the SC (15%), ST (7.5%) or OBC (27%). And that’s without taking into account the fact that this 28% is of total seats, while the caste-based reservations do not apply to all. | ||
| + | |||
| + | How did we get to this 28%? It’s based on a detailed analysis of fees for the MBBS course in over 530 MBBS colleges. About half the seats in private colleges, excluding deemed universities, are in the management quota or NRI quota. In the NRI quota, the average annual tuition fee is roughly Rs 25 lakh per annum. For the management quota, the average fees are around Rs 11 lakh though it varies from Rs 4 lakh in private colleges in West Bengal, which is uncommon, to Rs 18 lakh to Rs 20 lakh in states like Karnataka and Rajasthan. Besides the tuition fees, almost all colleges collect about Rs 2 lakh a year as charges for hostel, mess, exams, library and so on. | ||
| + | |||
| + | |||
| + | The most expensive seats are in the deemed universities. Over 8,500 seats in these universities constitute about 10% of all MBBS seats. Barely 3% or about 23,000 of the 7.7 lakh who qualified through the combined entrance exam, NEET, applied for these seats. The average annual tuition fees for NRI seats in these colleges are Rs 36 lakh, which is about Rs 1.6 crore for the entire course. The average fees for management seats in them are Rs 18 lakh. | ||
| + | |||
| + | TOI had reported earlier how the higher the fees, the poorer the average NEET score. The high fees leading to a virtual reservation for the rich has led to those with ranks even below 6 lakh in NEET getting admission, though there are only about 83,000 MBBS seats. | ||
| + | |||
| + | Even some government colleges, mostly in Gujarat (11 colleges) and Rajasthan (8 colleges) have management seats (1,350) and NRI seats (580) at an average Rs 18.5 lakh. The management quota seats in these government colleges range from Rs 7.3 lakh to Rs 18 lakh per annum in some of Gujarat’s municipal medical colleges in Gujarat. Others could also be as low as Rs 75,000 in Rajasthan to Rs 1 .3 lakh in Doon Medical College in Uttarakhand. | ||
| + | |||
| + | Most states governments have been pushing up fees in their medical colleges citing the high cost of medical education, though the money collected from increased fees is just a fraction of the budget. In Punjab, the cost of MBBS in government colleges went up from Rs 4.4 lakh to Rs 7.8 lakh, among the highest in the country. Fees in most government colleges in Maharashtra and Madhya Pradesh are about one lakh per year. | ||
| + | |||
| + | Incidentally, according to the latest expenditure survey done by the NSO in 2017-18, before the job loss of millions and economic devastation caused by the pandemic, the monthly expenditure of 80% of Indian families was less than Rs 10,500. Renowned economist Thomas Picketty had estimated that in 2015 about 5% of Indian adults earned over 63,000 a month or over 7.5 lakh a year. He estimated that just 1% (13.8 million) earned over 2 lakh. This is unlikely to have changed much since. What this means is that at best only 5% of families can afford the fees being charged for medical education in most institutions, even government ones. | ||
| + | |||
| + | Fifteen AIIMS accounting for about 1,100 seats offer the cheapest medical education, mostly charging Rs 1,628 or Rs 5,856 per annum. Centrally-funded institutions charge the least fees. West Bengal and Bihar offers the cheapest medical education in the country with the majority of colleges in the former charging Rs 9,000 as tuition fee and Rs 144 as hostel fees and the latter charging about Rs 6,000 as tuition fees and Rs 4,200-20,000 as hostel fees. Even among private colleges, West Bengal has among the lowest fees, mostly well below Rs 5 lakh for management seats and about Rs 15 lakh for NRI seats. | ||
| + | |||
| + | In 2016, the Parliamentary Standing Committee report on the functioning of the Medical Council of India (MCI) and medical education had strongly criticised “admission procedures which are primarily monetary based”. The committee recommended a common entrance test “to ensure that merit and not the ability to pay becomes the criterion for admission to medical colleges”. But with fees remaining unchecked, neither the new National Medical Commission nor the National Eligibility-cum-Entrance Test (NEET) has achieved this. | ||
[[Category:Bangladesh|MMEDICAL EDUCATION AND RESEARCH: INDIAMEDICAL EDUCATION AND RESEARCH: INDIA | [[Category:Bangladesh|MMEDICAL EDUCATION AND RESEARCH: INDIAMEDICAL EDUCATION AND RESEARCH: INDIA | ||
Revision as of 21:13, 7 March 2021

This is a collection of articles archived for the excellence of their content. Readers will be able to edit existing articles and post new articles directly |
All-India quota in deemed universities, govt. medical colleges
2017, May: To be filled by DGHS: SC
The Supreme Court has ordered that the all-India quota in deemed universities and government medical colleges will be filled by the director general of health services (DGHS) in New Delhi. This will include deemed universities run by religious and linguistic minorities too as these institutes have an allIndia character.
The quota is 15% for UG courses and 50% for PG courses. Till the year before last, deemed universities conducted their own exams and admitted all students.Last year, after losing a case in the SC in the middle of the admission process, they admitted students based on NEET rankings.
Common counselling for state quota seats in government and private medical colleges, including colleges institutions run by religious and linguistic minorities affiliated to state universities, shall be conducted by the state government or the authority designated by the state government. Moreover, state governments must conduct two rounds of centralised counseling for the all-India quota and process the admission too on behalf of deemed universities and private colleges.
The apex court has ruled that cheques for tuition fees should be collected by the state's admission-conducting body so that colleges do not state that candidates weren't turning up. After the second round of counselling for all-India seats, students who take admission should not be permitted to vacate them, the SC said.
“This would ensure that very few seats are reverted to the state quota and also allIndia quota seats are filed by students from the all-India merit list only. The students who take admission and se cure admission in deemed universities pursuant to the second round of counselling conducted by the DGHS shall not be eligible to participate in any other counseling,“ the SC ruled in a writ petition filed by Dar-us-salam Education Trust against the MCI.
The notification to be is sued by the state notifying the common counselling should also provide the fee structure of deemed universities and private medical colleges, as per the SC directive. “The students who secure admission in MBBS course pursuant to the common counselling conducted by the state government, should be made to deposit with the counselling committee the demand draft towards the fees payable to the institution. The admission counselling committee shall forthwith forward the demand draft to the respective institutioncollegesuniversity. The necessity for including the above-mentioned requirement has arisen as it has been time and again noticed that when students report to the college after the counselling they are refused admission by the colleges on some pretext or the other and it is shown by the college as if the student never reported to the college for admission.“
2017, Aug: 50% MBBS; 85% BDS seats at these institutes vacant
`Up to 12k seats may remain vacant', August 24, 2017: The Times of India
BDS Vacancies 85%; Admissions End On Aug 31
Deemed universities and private colleges across the country are staring at a huge crisis of unfilled undergraduate medical seats under the new system of centralised counselling introduced under the Supreme Court's orders this year.
As the third round of counselling comes to an end on Thursday , more than 50% of MBBS seats and almost 85% of dental seats in these institutes are still vacant.
The final mop-up of vacant seats is scheduled for August 28 (after 5 pm) and the admission process comes to an end on August 31. These institutes fear that a majority of their seats will remain unfilled as, under the new rules, these universities will not be allowed to admit students on their own.
Sources said even in government colleges nearly a third of the 15% seats under the all-India quota has remained vacant till now. However, unlike deemed universities and pri vate colleges, government institutions will get a chance to fill these seat as these will be transferred to the states. A senior health ministry official said the Directorate General of Health Services (DGHS), which is conducting the counselling, will seek legal opinion on how to resolve the crisis of unfilled seats.
While this may come as a ray of hope for medical aspirants, what is troubling the deemed universities is the new matrix of counselling, under which these institutes will have to go by the DGHS list even after the final transfer of seats. According to the head of a private medical col lege in Karnataka, “We have 200 MBBS seats, of which 30 are for NRIs. In this category, we have filled just one seat.Of the 170 general seats, 89 have been filled after DGHS counselling till the mop-up round. In BDS, we have filled 29 out of 100 seats.“ There are deemed universities where no admissions have taken place till now.
“After the mop-up round, which is getting over tomorrow, the seats will be transferred to the deemed universities. And for every 10 vacant seats, DGHS will release a list of 100 candidates (10 times higher). But when a similar process during the first three rounds has yielded next to nothing, we expect less than 10% of the vacant seats to be filled. Till last year, deemed universities had the option of choosing their students,“ said the vicechancellor of a deemed university in Hyderabad.
The admissions are being conducted based on NEETUG, 2017. “The counselling has been undertaken as per the apex court's order and guidelines, and no changes are possible to tackle the issue of unfilled seats. We are going to seek legal opinion and also approach the court again. Otherwise there is a possibility of up to 12,000 seats remaining unfilled this year,“ said a senior DGHS official.
Colour blindness
SC appoints expert committee to redefine bar
AmitAnand Choudhary, SC: Colour-blind ban for MBBS regressive, Mar 26 2017, The Times of India
Can a student suffering from colour blindness be allowed to pursue medical courses?
The Supreme Court has agreed to consider a plea of two students to open the door of medical colleges for them, saying the present practice of Medical Council of India not permitting colour-blind students to take admission in MBBS courses is regressive and should be done away with.
A bench of Justice Dipak Misra and Justice A M Khanwilkar appointed an expert committee of senior doctors to find out streams in which such students could be allowed. It said students with colour blindness were allowed to study medical courses in many other countries and the rules or guidelines followed in the country needed to be revived to allow such students to pursue co urses where colour blindness might not be a handicap.
“Total exclusion for admission to medical courses without any stipulation in which they really can practise and render assistance would tantamount to regressive thinking. When we conceive of global phenomenon and universal brotherhood, efforts are to be made to be within the said parameters. The march of science, apart from our constitutional warrant and values, commands inclusion and not exclusion,“ the bench said. The court directed Medical Council of India, the apex regula Council of India, the apex regulating body in the field of medical studies and profession, to constitute a committee of experts from genetics, ophthalmology , psychiatry and medical education from AIIMS and PGIMER, Chandigarh, to examine the issue. The court directed that the committee submit its report in three months.
The court passed the order on a plea of two medical students who were denied admission in college after clearing the entrance examination in 2015 as they were suffering from partial colour blindness. They had first approached TripuraHC which had turned down their plea, compelling them to approach the apex court.
Opposing the plea of stu dents, senior advocate Vikas Singh and lawyer Gaurav Sharma, appearing for MCI, contended that the decision to bar colour blind people was taken on the basis of report of an expert committee which held that people with such handicap would not be able to perform their duty as a doctor. They said a doctor would not be able to do fair diagnosis and prognosis of a disease as it depended upon colour detection Senior advocate K V Vishwanathan, who was asked to assist the court in deciding the issue, said a colour blind person may face difficulty in the stream of pathology , surgery, skin and general medicine but could efficiently perform in the field of psychiatry, social and preventive medicine. He said a complete ban on the admission to MBBS course would be violative of constitutional principle of equal opportunity and fair treatment.
’Colour vision deficiency should not be absolute bar:’Committee
A decades-old bar against colour blind people from becoming doctors is set to be removed with a Supreme Court-appointed committee recommending to the court that the current discrimination on the basis of colour vision deficiency (CVD) must be done away with.
Holding that the medical council of India (MCI) rule preventing colour blind people from taking up medical studies is “regressive“, the apex court had set up the committee in March this year, comprising experts from the fields of genetics, ophthalmology , psychiatry and medical education to review the regulation and analyse issues regarding CVD and the norms in other countries.
The committee, whose report has been filed by MCI's counsel Gaurav Sharma, agreed with the apex court's views and has said that CVD should not be an absolute bar as it is a common problem and did not significantly impact a person's ability to practise medicine. The report said there should not be any restriction either at the stage of admission, or at completion of study and registration as a medical practitioner.
“There are many reasons why doctors with CVD may perform as well as those with normal colour vision. Firstly , the diagnostic and treatment process is not solely reliant on the ability to perceive colours. There are many other cues from history of illness and examination that might be utilised to compensate for handicaps resulting from CVD. Doctors with CVD can also overcome their difficulties by carrying out a more thorough diagnostic assessment and taking the help of other colleagues,“ it said.
In its 35-page report, the committee said India is perhaps the only country where colour blind people are denied admission in medical colleges.CVD is not considered as a cri terion for rejection in US, UK and other western countries.
While setting up the committee, a bench headed by Justice Dipak Misra had said, “With the progress of science, expansion of many vistas of knowledge, inclusive culture, having regard to inclusive society and respect for differently-abled persons, it is obligatory on the part of MCI to take a progressive measure so that an individual suffering from colour blindness may not feel like an alien to the concept of equality .“
Severity of CVD might also be factored in while easing the bar for colour blind people as the report noted that “though the risk of medical errors may still exist, particularly among those with more severe CVD, the extent and seriousness of these errors is not clearly evident from the existing research“. “ As per current international practices, there is no policy of regulating entry of medical aspirants to study and practice of the medical profession based on colour vision deficiency . There are also no identified or mentioned practice restrictions,“ the report said.
The committee has noted that there is no identifiable compromise in the abilities of a clinical practitioner with CVD though certain tasks pertaining to specific fields of higher studies and super-specialisation might need closer evaluation. But colour corrective contact lenses or spectacles may be considered to assist the person, if and when necessary .
Commercialisation of medical education
1999-2019
Rema Nagarajan, June 9, 2019: The Times of India

From: Rema Nagarajan, June 9, 2019: The Times of India
How medical education became a business, one policy change at a time
Move to lift fee cap one more step towards commercialisation, say activists
The draft National Education Policy’s call for abandoning all regulation of fees in professional courses marks the latest in a series of steps that have aggressively pushed commercialisation of medical education over the last decade, say public health activists.
Till 2009, the official stance was that education could not be for sale or a for-profit venture. So on paper, all private colleges were run by trusts or charitable societies. Yet, the fact that many made illegal profits through capitation fees, hugely inflated tuition fees and other charges was an open secret. In February 2010, the then UPA government allowed companies registered under the Companies Act to open medical colleges though with the ironical caveat that “permission shall be withdrawn if the colleges resort to commercialisation”.
Even this fig leaf was dropped in August 2016, when then health minister JP Nadda approved an amendment in the eligibility criteria to allow companies to set up for-profit medical colleges. The government argued that no companies were coming forward to set up colleges because of the no-profit stipulation. It also argued that profits were in any case being made in nontransparent ways and that legally permitted profits would at least yield some income tax for the exchequer. There was little or no discussion about how students would be able to afford the huge fees charged in these colleges.
Following a huge outcry over spiralling fees in private medical colleges, a constitution bench of the Supreme Court had directed in 2003 that each state must have an independent fee fixation committee headed by a retired high court judge. A July 2018 Supreme Court judgment again upheld the 2003 judgment.
Mining giant Vedanta was one of the first companies to set up a college, in Palghar, Maharashtra. In a move that shocked the medical fraternity, students and activists, the state government gave it a free hand to decide fees. However, just a couple of months later, the college was found deficient and the Medical Council of India (MCI) refused to allow further intake in July 2018, a decision challenged by the company in Bombay High Court.
Allowing the entry of for-profit companies also led to those running societies or trusts asking why their own colleges could not to be converted into profit-making entities. In January 2017, the government acquiesced and notified that any medical college set up by an autonomous body, society or trust could be converted into a company, thus ending all pretence of medical education being a not-profit venture.
Going a step further, last month, the MCI Board of Governors amended the Establishment of Medical College Regulations, 1999 to allow consortia to set up medical colleges. A consortium, it clarified, could be a group of two to four eligible organisations including a society, trust, company, university or deemed university who have entered into a Memorandum of Understanding. The notification claimed that the object was to invite greater participation from the private sector in establishing medical colleges and “imparting high quality medical education and training facilities… without compromising the standards of medical education”. However, this move is viewed by many health activists as a way for private entities to use public hospitals to start medical colleges through MoUs with a “consortium”. Even before this, in several states including Maharashtra and Gujarat, public facilities had been utilised by private entities to set up medical colleges under the rubric of PPPs (public-private partnerships).
“All this is only about producing more doctors and not about the quality of doctors suited to our needs. Doctor shortage is in rural areas, but with no fee regulation only the affluent will become doctors. Will they serve where the shortage is?” asked Chhaya Pachauli, a public health activist from Rajasthan.
Dr T Sundararaman, former dean of the TISS School of Health System Studies, pointed out that over-production of doctors will suit corporates but not for the country. “Doctors will accumulate in urban areas leading to unhealthy competition and they will try to milk patients as is already happening in Mumbai. We need a policy that will get people to under-served districts of North and North East India,” he said.
While public health activists worry about the implications of a private sector without fee regulation, there is also the question of standards of medical education. India’s experience has been that regulation of private colleges has failed miserably, as both a parliamentary committee and the Supreme Court observed. What reason is there to believe things will get any better, ask the activists.
Capitation fees in govt. colleges
Rema Nagarajan, July 17, 2019: The Times of India
From: Rema Nagarajan, July 17, 2019: The Times of India
If you’re a resident Indian with poor NEET scores, getting admission in a government medical college is a pipedream, but if you are an NRI, you have a good shot at it. The reason is that it is not just private colleges commercialising medical education. Some state governments too have joined the bandwagon in the name of making their colleges self-financing. So, 3%- 15% seats are set aside for NRIs and some even have “management quotas”.
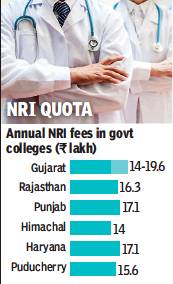
Five states — Gujarat, Rajasthan, Punjab, Haryana and Himachal Pradesh — and Puducherry have government medical colleges with NRI quotas. Unlike caste-based quotas, which are to compensate for historical deprivation and backwardness, the NRI quota is for being able to charge lakhs as fees. Most states claim the quota is to mobilise funds for maintenance and infrastructure, something that would earlier have come from the health budget.
Gujarat has the highest number of NRI seats at 241, followed by Rajasthan with 212, Punjab with 41, Puducherry with 22, Himachal with 20 and Haryana with 15.
NRI seats are open not only to NRIs but also those they sponsor. Thus, many can use this quota if they have a brother, sister or parent who is an NRI willing to give an undertaking to sponsor the entire course fee. If a student has no parents or is taken as a ward by near relatives, even NRI uncles, aunts or grandparents can be sponsors. There have been several cases of candidates faking eligibility, prompting greater scrutiny of candidates’ NRI claims.
A look at over 1,900 NRI candidates admitted in 2016 shows that almost three-quarters were unreserved category students, barely 3% belonged to SC/STs, and rest were OBCs. While the average NEET score of government quota students including reserved SC, ST and OBC seats in 2016 was 472.5, that of NRI candidates in private colleges was 220.8, and of those in government colleges was 339.6.
The NRI quota fees in government colleges range from Rs 14 lakh to almost Rs 20 lakh per annum. While this is very high compared to the fee charged for the other government seats in most of these colleges (Rs 25,000 to Rs 1 lakh per annum), it is much cheaper than the Rs 30 lakh per annum charged by most private colleges for NRI seats.
Earlier, Andhra Pradesh too had NRI seats in government colleges, but has discontinued this. Madhya Pradesh had about 28 NRI seats in government colleges till 2016 but discontinued the practice in the face of public protests. Last year, the Karnataka government had toyed with the idea of starting an NRI quota in government colleges, but dropped the idea after student outfits threatened agitations.
Former VC of Rajiv Gandhi University of Health Sciences and eminent cardiologist Dr K S Ravindranath explained that the reason for opposing NRI quota in Karnataka government colleges was because it would encroach on seats for poor meritorious students. The government ought to allocate more, but there are never sufficient funds to provide facilities for sports, research, simulation lab etc, he added.
N M Shrivastava, former joint director of medical education in MP, questioned the concept of using NRI seats to generate funds to improve colleges. “The money earned from NRI seats was small compared to the resources required to run a college. Moreover, government colleges are meant for public welfare, for poor to get free treatment and for meritorious students. They aren’t meant to make money. Free education is the government’s job in a democratic welfare state. That’s why the government decided to end NRI quota in MP,” he said.
With inputs from Bharat Yagnik in Ahmedabad, Initshab Ali in Jaipur, Shimona Kanwar in Chandigarh and Pushpa Narayan in Chennai
The societies model
July 17, 2019: The Times of India
The societies model
In Gujarat, ten out of 17 government medical colleges have NRI quota. Eight of these opened since 2011 were by the Gujarat Medical Education and Research Society (GMERS) formed by the state’s health ministry.
GMERS colleges’ quotas mirror those of private colleges with a government quota, a management quota and an NRI quota with annual fees of Rs 14 lakh.
NHL Municipal Medical College in Ahmedabad was set up in 1963 as an entirely municipality-funded college, but became self-financing in 2008-09. Surat Municipal Institute of Medical Education and Research, started in 1999, is also self-financing. Both charge NRI students close to Rs 20 lakh per annum. The Ahmedabad Municipal Corporation Medical Education Trust Medical College opened in 2009 too has an NRI quota.
In Rajasthan, 11 of the 15 government medical colleges have NRI quota. Like in Gujarat, the Rajasthan health ministry has formed the Rajasthan Medical Education Society under which eight new colleges opened since 2014 are self-financing. Apart from these, the government introduced 30 more NRI seats in three older colleges from this year — 15% of seats increased since 2014-15. The fees for NRI seats in the government colleges ranges from Rs 12.4 lakh in two colleges to Rs 16.3 lakh in the other nine.
Curriculum
2018: adultery, lesbianism are sexual offences
Rema Nagarajan, Adultery, lesbianism now sexual offences, November 14, 2018: The Times of India
The MBBS curriculum being revised after 20 years lists adultery and lesbianism as sexual offences in the section on forensic science, and in the one on obstetrics and gynaecology. Again, in the psychiatry section it puts transvestism in the list of “sexual perversions” and makes a reference to the Indian Mental Health Act, 1987.
Emergency medicine
Residency programmes as masters courses
Hospitals Get Cheap Labour, Medical Societies Moolah
Residency programmes in emergency medicine passing themselves off as masters courses have become a multi-crore industry .Many private hospitals running such courses charge Rs 11-19 lakh for a three-year course. Given the huge demand for doctors trained in the discipline, the industry finds no lack of takers.
Ironically , this ensures that the stipend or salary to be paid to these young doctors over these three years comes out of the course fees they pay. Sources in the private healthcare sector told TOI that this cheap or even free labour to run emergency departments is one of the biggest factors behind the increasing number of private hospitals offering these courses.
The masters in emergency medicine (MEM), administered by the George Washington University (GWU) in conjunction with several private hospitals is termed “a three-year postgraduate program in emergency medicine“ on the GWU website. The MEM being run by the Society for Emergency Medicine in India (SEMI), is promoted as a PG programme by most hospitals on their website, with only the fine print acknowledging it is not MCI recognised.
In the case of GWU-MEM, the affiliation is usually with the “academy“ that most corporate hospitals have, to train medical personnel needed for their hospital chain. Each GWU-affiliated academy or stand-alone hospital pays $60,000 to $90,000 (Rs 39 lakh to over Rs 58 lakh) per year to GWU for course administration and to cover the cost of the GWU faculty's monthly class visits. Each student pays Rs 4-6 lakh per year as fees and get paid about Rs 25,000 per month in the first year, going up to Rs 45,000 in the third year. In effect, the students get their stipend from the fees they pay and the hospital gets the free service of a bunch of doctors for three years.
GWU-MEM started in 2007 as a two-year fellowship.In 2010, a year after MCI recognised emergency medicine as a specialty and started the three-year MD course, the fellowship was converted into a three-year “masters“ programme. SEMI, whose board is dominated by doctors without an MCI-recognised PG medical degree, started its own MEM in 2011 in the name of Make in India.
SEMI took Rs 20,000 per year per student for course administration, much cheaper than the GWU-MEM. Stu dents also pay Rs 3,000 for SEMI life membership and about Rs 17,000 as examination fees. Thus SEMI's revenue from each MEM student is about Rs 80,000. With about 350 MEMs produced each year, that's about Rs 2.8 crore annually. The hospital running SEMI-MEM charges from Rs 75,000 to over a lakh per year as fees, again much cheaper than the GWU-MEM. SEMIMEM students are paid the same stipend as Diplomate of National Board (DNB) students (Rs 25,000 to Rs 50,000 depending on the state), claimed former SEMI president Dr T Srinath Kumar.
SEMI-MEMs have mushroomed across India as it is cheaper for hospitals and gives the same benefits in terms of getting a steady flow of cheap labour to run emergency departments.
SEMI earlier ran a one-year diploma course in emergency medicine, which has been wound up. GWU also used to run a one-year PG diploma. “If the idea was to address the shortage of doctors trained in emergency medicine quickly and to meet the rising demand, why would they extend the training to a threeyear masters programme?
Why not start more one-year diplomas or stick to two-year fellowships?“ asked a senior faculty of emergency medicine in a medical college.
With a huge mismatch in the number of MBBS graduates and recognised postgraduate seats, doctors who cannot make it through the entrance exam for MD and DNB in emergency medicine opt for these training courses even if they are unrecognised, as they help them get jobs in private hospitals. Societies like SEMI are glad to keep these lucrative courses running. Since emergency training courses include rotation to other departments including ICUs, hospitals are keen to get EM trainees they can use across departments. Some hospitals with just 60 emergency patients per day were training 14 one-year diploma students in emergency medicine along with 12 MEM trainees, raising questions about the quality of training. No one is opposed to training programmes as long as students are not cheated into believing their courses will get them a PG qualification that can be registered, and as long as the organisations running these courses do not claim their courses are equivalent to a recognised PG degree, pointed out Dr Praveen Aggarwal head of the department of emergency medicine at AIIMS.
Training courses in various specialties run by medical societies are common, but those do not claim to be a masters programme or degree.They are typically called certificate courses, fellowships or diplomas.
Ethics
2018: included in curriculum
Rema Nagarajan, Now, MBBS students to do course on ethics too, November 14, 2018: The Times of India
India has joined a long list of countries that have included a course in medical ethics as part of undergraduate medical education. The course will start from the first year of the MBBS programme and run until the final year.
The Competency Based Medical Curriculum uploaded on the Medical Council of India (MCI) website underscored the importance of ethical values, responsiveness to the needs of the patient and acquisition of communication skills through dedicated curriculum time for acquiring what it called “Attitude Ethics and Communication (AETCOM) competencies”. In the foreword to the curriculum, the Board of Governors currently running the MCI stated that medical students should be “trained to effectively communicate with patients and their relatives in a manner respectful of the patient's preferences, values, beliefs, confidentiality and privacy”.
Over the past four years, a panel of experts laid the basic framework for the revised MBBS curriculum. A book on AETCOM was prepared by the MCI and training of faculty on this module has been on since 2015. The curriculum set out the expectation from introducing the module stating that along with medical skills a medical graduate ought to be able to appreciate the sociopsychological, cultural, economic and environmental factors affecting health and develop a humane attitude towards patients.
According to the chairperson of the MCI Board of Governors Dr Vinod K Paul, emphasis on attitudes, ethics and communication was missing earlier as students mostly learned these from their peers, seniors and teachers. “By the 1990s, it had become obvious that ethics was important and most countries had introduced it in the medical curriculum. The framework of ethical decision-making is my shield to society when questioned about the decisions I take and doctors need to be taught how to wade through increasingly complex situations. Teaching AETCOM is a formal attempt to bring out the best in students. It will not change everyone, as students come with their own socializing and from different backgrounds. But the majority will benefit from it,” said Dr Paul.
Welcoming the introduction of medical ethics in the curriculum, eminent gastrointestinal surgeon Dr Samiran Nundy said the challenge would be to ensure that it was not restricted to didactic teaching and that it was relevant to India. “The most important thing is for the professors teaching ethics to practise what they preach. Students learn by emulating their teachers and so teachers must be seen doing what is right,” said Dr Nundy.
Dr Arun Gadre of the Alliance of Doctors for Ethical Healthcare, said the introduction of any ethics anywhere is good but felt that without role models in colleges, just teaching the theory of ethics would only make students cynical.
Foreign educated Indian doctors (FEIDs)
2012-14: Indian doctors with foreign medical degrees
The Times of India, Nov 06 2015
Sushmi Dey
China beats all to be biggest doctor factory for Indians
Not just Chinese consumer products, India also receives thousands of “made in China“ doctors. China is today the largest contributor of MBBS doctors to India followed by Russia, Ukraine and Nepal, according to data collated by the National Board of Examinations, which conducts Foreign Medical Graduate Examination (FMGE) screening tests. The FMGE is a voluntary entrance test introduced in 2002 as a qualifying exam for Indian students holding medical degrees from other countries and intending to practice medicine in India. The Medical Council of India (MCI) recognises this exam.
As many as 11,825 Indian students, who have Chinese MBBS degrees, took the FMGE test during 2012-2014, while 5,950 were from schools in Russia and 3,163 in Nepal. The rush for foreign destinations, experts say , is fuelled by those who fail to get admissions in Indian colleges. Of over 5 lakh Indian MBBS aspirants each year, about 4,500 get seats in government colleges.
While UK, Germany and Singapore attract candidates, the numbers are comparatively smaller than those who go to China and Nepal for European institutes are costlier. The number of doctors who train in countries like China and Russia has risen sharply in recent years, but they must clear the Foreign Medical Graduate Examination (FMGE) for provisional or permanent registration with Medical Council of India or any state medical council. There's an impression, however, that the calibre of doctors who train in these countries isn't on a par with those qualifying from Indian institutions.
The National Board of Examinations that conducts the FMGE ranks foreign universities or medical institutes on their candidates' performance in the screening test. While the government plans to increase PG seats in some super-specialty departments in a few key institutes, including AIIMS, there are no such plans for basic MBBS course.
Country of education, pass percentage

From: DurgeshNandan Jha, MBBS grads from abroad face a hard road to licence, October 1, 2018: The Times of India
Degree No Use Till They Clear Screening Test
It is unusual for medical graduates in India to be embarrassed around their relatives. But Kumar Gaurav, who completed his MBBS in March 2016, has not visited his Bihar hometown in two years. His relatives had once made fun of him because he couldn’t practice despite having a medical degree. And that had stabbed him right in his heart.
Gaurav went to a medical college in Nepal, but graduates from there can’t practice in India unless they clear the Foreign Medical Graduates Examination, a screening test conducted by the Medical Council of India twice a year. This applies to graduates from institutions in other countries as well, such as China, Ukraine, Russia, Bangladesh and the Philippines.
Fresh graduates return to India and join the ranks of those who have been trying to pass the test. It’s a tough life.
Chhattarpal Vasisth, who did his MBBS from Ukraine, is now enrolled in a coaching institute in South Delhi to crack the screening test. The 26-year-old comes from a small village in Haryana’s Bhiwani, and the first to be a doctor from there. “I could not get admission in government medical colleges. Private colleges charged over Rs 50 lakh. In Ukraine, it cost me less than Rs 20 lakh, including hostel fees,” he says.
Like Gaurav and Vasisth, more than 5,000 young men and women opt for medical degrees abroad every year because of low cost and ease of admission, among other reasons. China is the most popular destination, followed by Russia, Ukraine, Nepal, Kazakhstan and Bangladesh. Some even go to Pakistan.
The life that follows their return to India is different from what most anticipate. They also have to deal with the realisation that, hierarchically, they are considered less meritorious than homegrown medical graduates.
Gautam Nagar near AIIMS in Delhi is known for the large number of medical graduates and aspiring students who live there. Behind AIIMS are the lanes of Gurjar Dairy, an unauthorised colony where hundreds of medical graduates from abroad live in dingy accommodations, while enrolled in coaching classes and dreaming of cracking FMGE. “When I went to study in Ukraine, I assumed I would be more sought-after here on my return. Life was tough there. I lived on a tight budget and worked at restaurants,” says Dr Saurav Awasthi, an MBBS now employed at a government hospital in Delhi.
Med grads from abroad perform poorly in FMGE
People think we did not have the merit to study medicine but partied and came back with easy degrees. This is not true. Education standards there are better than most private medical colleges in India and even some government ones,” says Dr Saurav Awasthi, an MBBS, now employed at a government hospital in Delhi. He is a leading member of All India Foreign Medical Graduates Association, which works for the rights of students like him.
Their image is not enhanced by the fact that graduates from abroad perform poorly in FMGE. Between 2012 and 2014, graduates from Bangladesh performed the best, with 31% clearing the test. Then there are countries like Armenia and Kyrgyzstan, from where only 18% graduates make the cut. Each year, more than 10,000 appear for FMGE. In the June 2014 exam, only 5% passed. In June this year, the figure was slightly more encouraging: 26%.
Awasthi and others say the government should make the test compulsory for all graduates, including those from Indian colleges. Dr Yatish Aggarwal, an advisor to the National Board of Examination that conducts FMGE, points out, “A few years ago, following protests by foreign graduates over low pass percentage in FMGE, we asked some finalyear students from Maulana Azad Medical College and Vardhman Mahavir Medical College to take the test without prior notice. Nearly 80% of them qualified. Less than 20% of the foreign graduates made it.”
Recently, the health ministry issued directions that any Indian candidate wishing to pursue medical education from any foreign destination will have to pass the National Eligibilitycum-Entrance Test from now on.
2012-16: Poor ‘pass percentage’
The Times of India Jan 04 2016
The pass % of foreign medical degree holders in the screening test for recognition of their degrees in India is steadily declining. Student bodies complain about deliberately set tough questions to discriminate them against students from Indian universities.The examination bodies say that pass % is going down because of the increasing number of repeaters
2014-16: Poor performance in screening tests in India
The Times of India, May 25 2016
Pushpa Narayan
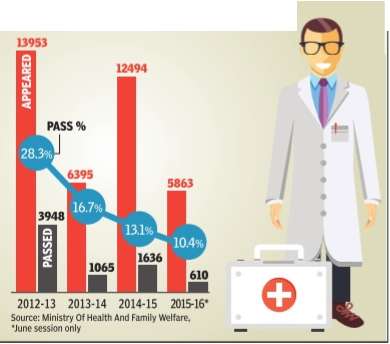
Statistics show students with medical degrees from foreign countries are finding it increasingly difficult to pass the screening test that allows them to practice in India.
The number of students taking the test has doubled but the pass percentage dropped from 50.12 in 2005 to 10.7 in 2015. In this period, the pass rate fluctuated around 20%, dropping to an all-time low of 4.93% in June 2014, when only 293 students passed. There has been an 80% drop, between 2005 and 2015, in Indian medical graduates from foreign universities passing the mandatory screening test that the National Board of Examinations holds.
According to the Indian Medical Council Act, 2001, citizens with undergraduate degrees from outside India should clear the screening test conducted twice every yearJune and Decemberbefore they do a one-year in ternship in one of the MCIrecognised medical colleges.One has to score 50% to clear the test. Students say the the test is extremely tough.“Most questions are from postgraduate medical tests,“ said Raghuram Nayak, who completed his graduation in Ukraine in 2012. The students' association of foreign medical graduates say the board has made the test difficult to discourage students from going abroad and opt to study in private colleges here that charge as much as Rs 1 crore.
These students aren't even considered graduates in India unless they pass the test. “ Many of students spend lakhs in coaching centres to clear the test,“ said Raghuram. Officials at NBE deny these.
An expert committee which studied 11 question papers from 2013 to 2015 submitted a report to the ministry of health stating that 52.78% of the questions were of “low difficulty“ and 42.22% questions were of “moderate difficulty“. Board executive director Dr Bipin Batra said the test had no negative marking and most students find it difficult because public health priorities of other nations are different from ours.
2016-17: 74% rise in Indians seeking foreign degrees
Sushmi Dey, December 18, 2018: The Times of India

From: Sushmi Dey, December 18, 2018: The Times of India
Number of students aspiring to study medicine abroad is rising rapidly with applications from such candidates increasing by 74% in just one year between 2016-17 and 2017-18, official data show.
The Medical Council of India (MCI) received 18,383 applications in 2017-18 for the mandatory eligibility certificate required so far from the medical education regulator to study medicine abroad, as against 10,555 applications in the previous year, as per information given by MCI in response to an RTI application.
MCI issued a total of 14,118 eligibility certificates in 2017-18, compared to 8,737 in 2016- 2017.
Experts say while the number of medical seats are limited in India, increasing awareness about foreign institutes coupled with their affordability has resulted in more aspirants seeking admissions abroad.
“Information provided in the RTI speaks volume on the shift in medical education trends. The key reason for this is the lack of medical seats in India. Apart from this, higher awareness levels of the overseas colleges, more affordable fees compared to Indian private colleges, curriculum aligned to international standardsetc. are other reasons why students prefer to study MBBS abroad,” says Saju Bhaskar, president & founder of an overseas medical university, Texila American University.
However, there are concerns in the Indian medical fraternity that the trend will impact the quality of doctors coming to practice in India. “Quality of medical education in India is one of the best in the world. However, since the number of seats are limited and candidates have to qualify a tough test, other countries like Russia, China and Eastern Europe provide an easy path, mainly for those who can pay,” says Dr Gurinder Grewal, former president, Punjab Medical Council.
Around 12 lakh aspirants take NEET for undergraduate medical course every year. Out of this, around six lakh clear the exam for about 68,000 MBBS seats. The rest try for dental and Ayush (Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy) courses. Many of these candidates, who fail to qualify NEET, also pursue medical education abroad, mainly in countries where they can seek admission with entrance examination.
Medical colleges
2017: states where concentrated; private/ government
March 31, 2018: The Times of India

The number of private Medical colleges vis-à-vis government Medical colleges.
All figures presumably relate to 2017
From: March 31, 2018: The Times of India
See graphic:
The 7 states where Medical colleges are concentrated;
The number of private Medical colleges vis-à-vis government Medical colleges.
All figures presumably relate to 2017
2018: the best and worst served states
Rema Nagarajan, June 18, 2019: The Times of India

From: Rema Nagarajan, June 18, 2019: The Times of India
Jharkhand last got a ‘new’ medical college 50 years back
Can you believe that there is a state that hasn’t had a single new medical college opening in half a century? The last medical college to open in Jharkhand was the government-run Patliputra Medical College in Dhanbad in 1969, long before the state even came into existence. There are just two more medical colleges in the state, both government-run, opened in 1960 and 1961. Jharkhand also happens to be the state with the worst doctor to population ratio of close to one for every 8,200 people.
In spite of this, even in 2019, the year that witnessed the largest ever expansion of medical seats, especially government seats, Jharkhand did not get a single new college. About 231 medical colleges have been opened across India since 2010, yet not one in Jharkhand. An AIIMS has been sanctioned for Deoghar in the state, but that’s still in the pipeline.
Chattisgarh is another state with an abysmal doctor-population ratio of 1:4,338. Yet, it too got no new colleges in the 2019 mega expansion. Bihar, with a doctor-population ratio worse than 1:3,200 got just one new private college. Thus the three states worst off in terms of doctorpopulation ratios have been largely ignored even in the current year. Unlike Jharkhand, however, Chhattisgarh has added seven new colleges since 2010, four of which were government run, though two of these seven have been debarred from admission this year. Bihar too has added six new colleges from 2010, including four government ones with 100 seats each.
Other states with poor doctorpopulation ratios such as Uttar Pradesh, West Bengal and Madhya Pradesh got seven, four and three government colleges respectively, each with 100 seats in the 2019 expansion. Even states which already have a glut of doctors, like Tamil Nadu with one doctor for just over 250 people, got two new colleges, one private and one government owned, with 150 seats each. From 2010 onwards, medical colleges and MBBS seats have increased substantially, especially in the government sector. Every big state, including those complaining of over-production of doctors has continued to open new medical colleges barring Jharkhand. Uttar Pradesh saw the greatest increase with the addition of 29 colleges taking the total number to 55, second only to Karnataka with 59 colleges. The state has only one doctor for every 3,767 persons. Interestingly, Karnataka, which already had among the highest number of medical colleges, saw 19 more being opened from 2010, of which 10 were private with 150 seats each. Of these 10 new private colleges, five have been opened in Bengaluru, which already had seven. Two of the nine government colleges set up since 2010 are also in Bengaluru, taking the total in the city to 14. Karnataka’s doctor-population is 1:507, well above the WHO target of 1:1,000.
Tamil Nadu has added 13 colleges since 2010, of which seven were government colleges. It now has a total of 49 colleges, not counting nine in adjoining Pondicherry. Kerala, which is also facing a glut with one doctor for about 500 people, added four government colleges with 100 seats each and seven private one with 150 seats each in the current decade. The net result is that some states are facing a steadily worsening glut of doctors while others are facing desperate shortages that are not getting addressed.
2018-19: government vis-à-vis private colleges

From: March 12, 2020: The Times of India
See graphic:
Management-wise colleges and enrolment, 2018-19
Neglect of medical education
1 govt med college seat for 55k people
Massive Shortage Of Seats Allows Private Sector To Jack Up Education Cost
Rema Nagarajan | TIG
The Times of India 2013/08/12
Shortage of doctors
The shortage of doctors in India can be blamed on the government neglecting medical education for three decades from 1970 till 2000. In a 15-year period from 1951 to 1966, sustained investment in medical education led to India having one medical seat in a government college for roughly every 37,000 persons, down from one for every 71,000 in 1951.
Over the 47 years since then, the situation has worsened dramatically with one government medical college seat for over 55,000 today. This has resulted in the private sector taking over medical education in a big way. That, in turn, has meant spiralling costs, question marks over quality and a sharp geographical skew. Even with the private sector included, India now has one MBBS seat for every 26,042 people, only a small improvement from one for every 33,521 in 1966. In contrast, the period from 1951 to 1966 had seen the ratio cut by more than half.
A look at the data on medical seats and colleges available with the Medical Council of India (MCI), the regulator for medical education and doctors, shows that the availability of medical seats has improved in recent years. Almost half (47%) of the available seats have been created since 2000. However, 72% of the seats added since 1970 are in the private sector.
Why should this be a matter of concern? There are several good reasons for this to be cause for worry. For starters, private medical education is expensive making it inaccessible for most Indians. In private colleges, the cost of graduating is Rs 15 lakh-40 lakh or more, not including capitation fees. In a government college, it ranges from a mere Rs 10,000 as tuition fee in Delhi’s Maulana Azad Medical College for the entire MBBS course to about Rs 1.5 lakh in Trivandrum Medical College, one of the more expensive government medical colleges.
The quality of education in private medical colleges, too, has been a matter of great concern as they are less transparent and have proved difficult to regulate. The fact that many are owned by political heavyweights does not help.
The lost states, the lost decades
The private sector has also led to a geographical skew in the distribution of seats. Over half the private sector seats are concentrated in just four states—Karnataka, Tamil Nadu, Andhra and Kerala—though they account for just 21% of India’s population. In Karnataka, for every government seat, there are almost four private medical seats, while in Kerala there are two private seats for every government seat. However, in the poorer states like Bihar, UP, West Bengal, Rajasthan, Assam, Jharkhand, Chhattisgarh, and in the northeast, medical education remains largely dependent on government medical colleges. In most of these states, no new government medical colleges were created for decades between 1960s and 2000. In over two decades following Independence, the government created 69 medical colleges with over 8,500 seats. This was followed by three decades (1970-99) of utter neglect, when the population almost doubled from 548 million to over a billion, while the government added barely 2,000 more medical seats. The surge of the private sector started in the 80s as government investment in medical education declined drastically, but it has accelerated since the turn of the century.
After the government woke up to the crisis in medical education and took steps to increase government investment and also relaxed the norms for running a medical college, there has been a surge in the number of medical colleges, both public and private, especially in the last three years.
Aformer member of the Board of Governors of the MCI, Dr Ranjit Roychoudhury, had this to say: “We lost three decades starting from the 70s. The government stepped back from medical education thinking that the private sector would be able to fill in. At the time, the problems of private medical education were not envisaged, such as the question of inequity, quality of education and the geographical skew. We are now trying to rectify this problem.”
2000-2013
Since 2000, the government has created 9,300 medical seats, almost as many as it did in half a century from 1950 till 2000. But the 9,300 seems a pittance compared to the 17,700-plus private sector seats created in the same period. Almost 60% of the latter were in four southern states. In 2013, for the first time since 1975, the government has created more medical seats than in the private sector. In 2013, Centre created 1,300 seats in 14 new colleges. Another 3,013 have been added to existing colleges. Thus, in just this year, the government has created twice as many seats as it did in 30 years from 1970 to 2000. Is the trend finally changing for the better? Let’s hope so.
Nursing colleges
INC cannot recognise nursing colleges: HC
INC not authorised to recognise nursing colleges: High Court, July 25, 2017: The Hindu
Council told not to webhost material indicating institutions require its recognition
The High Court of Karnataka on Monday declared that the Indian Nursing Council (INC) has no authority to grant recognition to institutions imparting nursing courses. It restrained the INC from publishing on its website material indicating that the institutions have to obtain recognition from it.
The court held that the council is empowered to prescribe qualification and syllabus for nursing courses, and not to accord recognition to colleges.
Justice L. Narayana Swamy delivered the verdict while allowing petitions filed by the Karnataka State Association of the Managements of Nursing and Allied Health Sciences Institutions, and some nursing colleges.
Also, the court said that all such stands withdrawn from the INC’s website forthwith.
The action of the INC claiming that nursing colleges have to get recognition from it, publishing the list of recognised colleges, and releasing any such material on its website, would cause hardship to petitioners and nursing colleges as students, who visit the website would infer that colleges which are not in the list, are not recognised.
‘Against the law’
The action of the INC in publishing the list of recognised nursing institutions is against the law declared by the High Court in a earlier case of 2005 as well as an order of the Supreme Court, Justice Narayana Swamy observed in the order.
The petitioner-association had claimed that the INC has no authority to grant recognition to institutions imparting nursing courses, such as auxiliary nurse and midwife, general nursing, B.Sc. Nursing and M.Sc. Nursing, after the INC removed Karnataka’s nursing colleges from the list of recognised institutions of nursing.
The association had supported the State government’s notification of December 14, 2016, which was issued citing 2005 order of the High Court, clarifying that the power to grant recognition, impart training in nursing and fixation of intake vests with the State government, the Karnataka State Nursing Council and the Rajiv Gandhi University of Health Sciences and not the INC.
Prior to the December 2016 notification, the State had insisted recognition from the INC.
Petitions rejected
Meanwhile, the court rejected the petitions filed by Student Nurses’ Association of the Trained Nurses’ Association of India and several other nursing colleges seeking a direction to the INC to renew or grant recognition to the nursing institution, while claiming that it is the INC that has to grant recognition to their qualification if their nursing certificate or degree is required to have recognition across India and abroad.
PG Medical courses
Admissions only on merit: SC
The Times of India, Jan 13 2015
Admissions to PG medical courses only on merit: SC
Admissions to post-graduate medical courses can be done only on the basis of merit of students appearing in the entrance examination, the Supreme Court said while quashing Kerala government's decision to reserve seats for doctors working in its hospitals and other departments. The apex court said the state overstepped its jurisdiction by making a law earmarking 40% of total seats available to the state quota for its medical officers who were to get admission on the basis of their seniority , without appearing in the entrance examination.
A bench of Justices T S Thakur and R Banumathi said regulations framed by the Medical Council of India were binding and state governments could not make any rule in violation of the regulations. “Regulation 9 (of MCI) is, in our opinion, a complete code by itself inasmuch as it prescribes the basis for determining the eligibility of the candidates including the method to be adopted for determining the inter se merit which remains the only basis for such admissions. To the performance in the entrance test can be added weightage on account of rural service rendered by the candidates in the manner and to the extent indicated,“ it said.
The court said the method, however, was given a go-by by the impugned legislation when it provided that in-service candidates seeking admission in the quota shall be granted such admission not on the basis of one of the methodologies but on the basis of seniority of such candidates.
Change in rules for those with disability/ 2018
PG med admission: Change in rules for those with disability, March 22, 2018: The Times of India
The health ministry has granted approval to amend the rules for admission of people with disabilities in postgraduate medical courses to help them get the benefits of reservation, according to an official statement.
The percentage of seats to be filled by people with disabilities has been increased from 3% to 5% in accordance with the Rights of Persons with Disabilities Act, 2016, the statement said. Union health minister JP Nadda termed it a “historic” decision. “Now all with 21 benchmark disabilities as per the Rights of Persons with Disabilities Act, 2016, can register for admission to medical courses,” he said. According to the amended provisions, the disabilities include hearing impairment, locomotor disability, dwarfism, intellectual disability, autism, cerebral palsy, multiple sclerosis and thalassemia.
50% institutional preference for PG medical seats
Banaras Hindu University (BHU) and Aligarh Muslim Univesrity (AMU) will stand together on the same side in the Supreme Court to challenge an Allahabad High Court order doing away with 50% institutional preference in admission to PG medical seats.
BHU and AMU, both central universities, are relying on the Supreme Court's 2003 judgement in the Saurabh Chaudri case laying down the guidelines for filling up of PG medical college seats in government colleges. The SC had held that 50% of the seats would be reserved for all-India quota to be filled through a common entrance test. The government medical colleges could give preference to candidates from their own institution to fill the balance 50% seats in post-graduation courses.
On a PIL, without making the BHU or AMU a party, the HC had opened the 50% institutional quota seats in PG medical courses in these two central universities for students from any medical college in UP based on their ranking in National Eligibility cum Entrance Test (NEET).
“The implication of the HC order is that the admissions to the MD, MS and MDS courses in BHU as well as AMU, which has already been finalised and completed for the year 2017, has been rendered void. The HC did not offer any opportunity to the petitioner university to establish justify the validity of 50% quota available to the university under the institutional category,“ the BHU said and sought an interim stay of the HC order.
PG courses: weightage for rural service
NEW DELHI: The Supreme Court said on Wednesday that a doctor who forgoes urban comforts to serve in rural areas could not be denied the consequent weightage for admission to PG courses in government medical colleges of any state just because he obtained the MBBS degree from another state.
A bench of Justices Ashok Bhushan and Deepak Gupta set aside an order of the Allahabad high court, that granted preference in admission for PG courses to those in-service doctors who rendered rural service in UP after graduating from a medical college of the state.
The bench said: "Once graduate doctors, whether they cleared their MBBS or BDS examination from within UP or from any other part of the country, are selected and join the medical health service in UP, they form part of one service - Provincial Medical Health Services. Thereafter, when these doctors are posted to remote or difficult areas, they are posted as doctors of PMHS and not on basis of the state from where they did their graduation."
With this ruling, an MBBS passout from any state can join rural health services in another state and still be able to avail of the weightage, an additional 10% of marks per year of rural service up to a maximum of 30%, for admission to PG courses in the state where he rendered rural services.
The SC also set aside another direction of the Allahabad HC which had annulled the institutional quota of up to 50% of seats in PG medical courses of Aligarh Muslim University and Banaras Hindu University and directed filling up of these seats from among candidates who have passed MBBS from institutions, universities and colleges in UP.
SC sets aside HC order on institutional preference
Jun 7, 2017: The Times of India
SC sets aside Allahabad HC order on PG medical seats
NEW DELHI: The Supreme Court set aside the Allahabad High Court's May 29 order which had quashed 50 per cent institutional preference in admission to PG medical seats.
A vacation bench comprising Justices Ashok Bhushan and Deepak Gupta said institutes like the Banaras Hindu University (BHU), Aligarh Muslim University (AMU) and the government-run medical colleges in UP will continue conducting counselling and fill up the seats by June 12.
The high court on May 29 had passed order allowing to fill up the 50 per cent institutional quota seats in PG medical courses in these two central universities and other government-run univerities for students from any medical college based on their ranking in NEET.
The apex court order came on the plea of BHU and AMU contending that the high court verdict was violative of earlier apex court judgement and Medical Council of India (MCI) regulations which allow institutes to take admissions on 50 per cent seats from their own institution.
Both these central universities had got the support from the MCI, which had argued that the high court has erred in interpreting the laid down regulations. Additional Solicitor General Maninder Singh, appearing for BHU, had sought immediate stay of the high court's order saying the "entire apple cart" cannot be reversed. Senior advocate Salman Khurshid, appearing for the AMU, had said some students have already been admitted by the varsities under the 50 per cent quota, therefore the high court verdict needs to be stayed.
SC finds serious flaws in HC’s order
AmitAnand Choudhary, Med admissions: SC rips into HC’s order, November 26, 2017: The Times of India
The permission given by a division bench of the Allahabad high court to a Lucknow-based medical college to admit students just three days after the Supreme Court rejected the plea has elicited a strong reaction from the apex court, which called it a case of “judicial indiscipline” as it minced no words to reprimand the judges for violating judicial propriety.
A bench of CJI Dipak Misra and Justices A M Khanwilkar and D Y Chandrachud expressed “shock” and slammed the judges for passing an order “for some unfathomable and inscrutable reason”, a deviation which has the “potentiality to take justice to her coffin”.
‘HC move shows unjustified haste’
It is a most unfortunate situation that the division bench has paved such a path. One cannot but say that the adjudication by the division bench tantamounts to a state as if they dragged themselves to the realm of ‘willing suspension of disbelief’. Possibly, they assumed that they could do what they intended to do,” the SC bench said.
“A judge cannot think in terms of ‘what pleases the prince has the force of law’. Frankly speaking, the law does not allow so, for law has to be observed by requisite respect for law,” it said.
The bench noted that the Supreme Court had, on August 28, restrained the high court from passing any interim order in favour of the medical college for the current academic year while allowing the institution to withdraw its petition.
The high court, however, allowed the college to admit students for the 2017-18 batch on September 1withoutwaiting for a response from the Centre and the Medical Council of India.
“It is clear as the cloudless sky that the judgment of the high court shows unnecessary and uncalled-for hurry, unjustified haste and an unreasonable sense of promptitude possibly being oblivious of the fact that the stand of the Medical Council of India and the central government could not be given indecent burial when they were parties on record. Such a procedure cannot be countenanced in law,” the apex court said.
“The content of the August 28 order is graphically clear. The HC was not allowed to pass any interim order pertaining to the academic session 2017-18 but the division bench of HC, for some unfathomable and inscrutable reason, referred to certain judgments of this court and allowed the prayer. It is beyond our comprehension as to how the high court could have even remotely thought of passing an order granting the letter of permission for the academic session 2016-17 and renewal for 2017-18,” it said.
The apex court said: “It is necessary to add and repeat that the division bench had no reason to abandon the concept of judicial propriety and transgress the rules and further proceed on a path where it was not required to. Such things create institutional problems and we are sure that the judges shall be guided by it.”
The bench noted that the SC had restrained the HC from passing any interim order in favour of the medical college in Lucknow
One cannot but say that the adjudication... tantamounts to a state as if they dragged themselves to the realm of ‘willing suspension of disbelief’. Possibly, they assumed that they could do what they intended to do. It has the potentiality to take justice to her coffin
— SC BENCH on HC judges
Many hospitals with PG seats don’t meet standards/ 2017-19
Rema Nagarajan, May 11, 2019: The Times of India

From: Rema Nagarajan, May 11, 2019: The Times of India
Fake faculty, fake patients, inadequate infrastructure — these grievances are common about private medical colleges. They are now cropping up in complaints against private hospitals accredited by the National Board of Examination (NBE) for post-graduate seats. Yet, when a student complained about one such institution, the board responded saying that the hospital authorities “confirmed that they are following all the norms, rules and regulations set by NBE” and hence the matter was being closed. There was no investigation or inspection to check whether the complaint had merit. The assurance of the accused was enough for the matter to be closed. This despite the fact that there have been several cases of hospitals shutting shop or DNB (Diplomate of National Board) programmes having to be shut down for not complying with the minimum requirements to run the programme. In most cases, NBE had to relocate the stranded students to other hospitals. In 2018 alone, DNB programmes in 12 institutions accounting for 44 seats in various disciplines had to be shut down and 50 students had to be relocated. In 2017, three DNB programmes accounting for seven seats had to be discontinued. Mercifully, no students had to be relocated as there were none.
No programmes were shut down in 2015 and 2016. “Since there was no governing body in 2015 and half of year 2016, no decisions were made regarding withdrawal of accreditation,” said an NBE spokesperson. With no governing body, students’ complaints went unresolved forcing many of them to drop out of DNB programmes. NBE regulates DNB, a post graduate qualification like MD/MS. DNB seats are mostly in private hospitals or institutions accredited by the NBE after an assessment to ensure that they have the required infrastructure, patient load and faculty. Single specialty hospitals must have at least 100 beds and multi-specialty hospitals at least 200 to be eligible for a DNB seat. However, DNB students in several hospitals have complained about not even 100 beds actually being available and asked the NBE to do surprise inspections.
“Unlike MCI, which puts up assessment reports of medical colleges in the public domain, the NBE refuses to do so. Hence students have no way of knowing what kind of an institution they are joining or what infrastructure the institute claims to have. Shifting students to other cities in the middle of a course causes much hardship,” said Dr Teena Gupta, National Secretary of the Association of DNB Doctors.
2018: MRCP, 4 other countries’ PG equal to Indian PG
Royal College Membership Only An In-Training Exam, Not A Qualification
Membership of the Royal College of Physicians of the UK (MRCP-UK) is only an “intraining examination” and not a qualification for recognition as a consultant in the UK. However, it is being considered as equivalent to an MD, MS or DM in India — all postgraduate degrees that qualify a person for consultant status — after the Medical Council of India issued a notification in March 2017 that postgraduate qualifications awarded in five countries including the UK would be treated as equivalent to these Indian degrees.
Since then, several private hospitals have started offering MRCP stating that it is equivalent to postgraduate medical degrees in India. However, responding to TOI’s queries, Professor David Galloway, president of the Royal College of Physicians and Surgeons of Glasgow clarified that MRCP is an “intraining examination” that is “set well below the level required at completion of specialist training”. The MCI is currently re-examining the issue of equivalence of MRCP and a final decision in the matter is awaited.
In India, the MRCP is promoted as a three-year structured post-graduate programme with core medical training (CMT) being offered in partnership with the Joint Royal College of Physicians Training Board. According to the MRCP-UK international brochure, the three-part MRCP(UK) merely makes a person eligible for higher specialist training.
In India, only an MBBS doctor with post graduate degrees like MD or MS can become a specialist or consultant. In the UK, as Galloway pointed out, “a CCT is required to gain a UK consultant position”. Certificate of completion of training (CCT), which takes five years, shows that a doctor has completed an approved specialist training programme and is eligible to become a consultant in the National Health Service in the UK. He added that the CCT is a very different standard and should not be compared to the MRCP.
Dr Galloway also clarified that the CMT being offered as part of MRCP courses in India was not the same as CCT. CMT refers to core medical training, that is early years post graduate training, and it is just part of the full general internal medicine curriculum of five years, he said.
Thus, a qualification that is not even considered a postgraduate degree in its home country is being considered so in India and equivalent to MD/MS for appointment to the post of assistant professor in medical colleges.
In the case of MBBS degrees given by foreign universities or institutions, the MCI stipulates that it has to be a recognised qualification for enrolment as medical practitioner in the country in which the institution awarding the qualification is situated. Only if this is true does the MCI grant the eligibility certificate that is required for taking the screening test that foreign medical graduates must clear to be allowed to practice in India. Yet, this principle does not seem to have been applied to the MRCP-UK with CMT.
In India, only an MBBS doctor with PG degrees like MD or MS can become a specialist or consultant. However, in the UK , ‘a certificate of completion of training is required to gain a UK consultant position’
Physically handicapped quota
SC: students with low vision can get admission
After paving the way for the colour blind to pursue medical studies, the Supreme Court has now allowed aspiring medical students suffering from low vision to get admission, saying the present law did not bar them from becoming a doctor.
A bench of Justices Arun Mishra and Indira Banerjee came to the rescue of an Ahmedabad-based student who was denied admission in a medical college despite qualifying NEET 2018 with a rank of 419 in the physically-handicapped category.
The court brushed aside the contention of MCI that persons with visual impairment of 40 per cent or more could not be admitted to undergraduate medical courses and the beneficial provision of the Rights of Persons with Disabilities Act, which provides reservation for the differently-abled, could not be invoked in MBBS/BDS courses.
State govt. has power to adjudge suitability of candidate
Merit of disabled candidate not sole key for MBBS seat: HC, August 22, 2018: The Times of India
The Gujarat high court rejected a petition by three disabled students seeking admission in MBBS under physically handicapped quota. The court said the candidate may be meritorious, but the state government has the power to adjudge suitability of a physically challenged person to pursue medical studies.
Ganesh Baraiya, Muskan Shaikh and Hina Mevasiya had approached the HC after the medical board and an appellate authority rejected their case that they are suitable to pursue MBBS. Ganesh was declared 72% disabled with a 109 cm height, while Muskan’s amputated hand left her 75% disabled. Hina was declared 50% disabled due to paraplegia. Their petition cited the Right of Persons with Disabilities Act which states that all persons with a physical disability between 40% and 80% are eligible for admission in medical courses.
Private medical colleges
Can't have own entrance test
The Times of India, Mar 9, 2016
Yogita Rao
The SC move is aimed at checking deliberate suppression of vacancy position in PG seats by the states.
The Supreme Court dismissed a plea by the association of Maharashtra's private medical colleges to be allowed to conduct its own common entrance test (CET) for medical and dental college admissions. It means students will be admitted to state as well as private colleges on the basis of a single test conducted by the state CET cell.
The Maharashtra Unaided Private Professional Educational Institutions (Regulation of Admission and Fees) Act, 2015, that lays down the state CET clause, was challenged by the Association of Managements of Unaided and Private Medical and Dental Colleges in the Bombay HC in August 2015, and the case finally reached the SC. Though this petition was meant only for the medical postgraduate entrance test, the order is being seen as precedence for all other entrance tests that will be conducted by the state under the provisions of the new act.
A petition challenging the law itself is still pending in the HC. Association chairman Kamal Kishore Kadam said the apex court has asked them to wait for the outcome of the main petition, challenging the law. "We will see if it is possible to file a fresh petition in the HC. The government is taking away several powers given to us by a past SC order. They do not give us any money to run the institutes, how can they seek control over them?" asked Kadam. "Some of our institutes are ready to run into losses, but we will not fill our seats with students allotted by the state government," he added. A potential standoff seems brewing with a government official saying the state may act against institutes that refuse to admit students allotted by the competent authority as per the provisions of the existing act.
Counselling by private colleges banned
AmitAnand Choudhary, SC bans counselling by pvt med colleges, Sep 23 2016 : The Times of India
`Process To Be Carried Out By States'
After setting out implementation of the national eligibility cum entrance test (NEET) as the single window exam for admission in all medical colleges, the Supreme Court said on Thursday that private medical colleges cannot conduct counselling for admission to MBBS and BDS courses.
The admission process, the court said, would be done through centralised counselling conducted by the state governments concerned.This means that educational institutions will not be able to reach out to prospective students through “offer letters“ on the basis of NEET results.
The court passed the order on a petition filed by the Madhya Pradesh government seeking contempt proceedings against private colleges which, it said, were defying the SC order by holding their own counselling for admission in MBBS and BDS courses. The order has wider application as private colleges in other states are also conducting counselling which has been challenged in the court.
“If any counselling has been done by any college or university and any admission has been given so far, such admission shall stand cancelled forthwith and admission shall be given only as per centralised counselling done by the state government,“ a five-judge Constitution bench said. The SC, however, refused to pass any punitive order against the colleges on the contempt plea and allowed them to send their representatives to participate in the counselling process.
Fees
2016: sharp increase
Capitation fees gone; private colleges’ fees zoom up/ 2016 Capitation fees out, pvt medical colleges hike tuition charges, Sep 26 2016 : The Times of India TEAM TOI-HEALTH
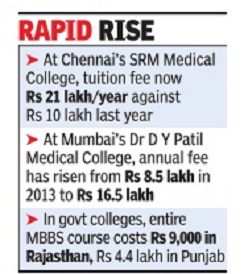
The Times of India
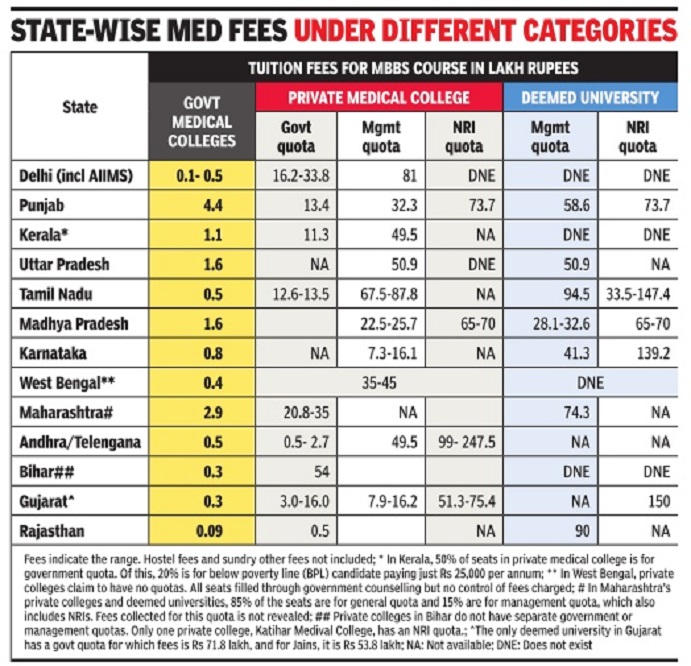
The Times of India
With the National Eligibility-cum-Entrance Test (NEET) becoming a hurdle to charging capitation fees, private medical colleges across India have substantially hiked tuition fees, while the cost of medical education in government colleges remains the same.
Tamil Nadu saw the highest jump in cost of private medical education. At Chennai's SRM Medical college, the tuition fee is now Rs 21 lakh a year or Rs 94.5 lakh for the four-and-a-half year MBBS course, against Rs 10 lakh per annum last year. This does not include expenses on books and lodging.
In Katihar Medical College in north Bihar, the annual tuition fee has been revised from Rs 8 lakh to Rs 12.5 lakh. In Delhi, at the Hamdard Institute of Medical Sciences, tuition fees in the management quota is up from Rs 15 lakh to Rs 18 lakh.
In government colleges, the sums range from as little as Rs 9,000 for the entire MBBS course in Rajasthan to Rs 4.4 lakh in Punjab. While most private medical colleges come under the purview of the Supreme Courtappointed fee committees in each state, deemed universities rarely come under the states' radar, leaving room for them to arbitrarily fix fees -a trend seen across the country . At Dr D Y Patil Medical College, Navi Mumbai, for example, the official fee is hiked by 3% every year. In 2013, the annual fee stood at Rs 8.5 lakh. This year, it's up by 32%. Students now have to pay Rs 16.5 lakh annually or Rs 76.2 lakh for their entire course. Similarly , at Chennai-based Saveetha University, the annual tuition fee has gone up from Rs 9 lakh last year to Rs 15 lakh now.
Private universities say their overheads have been very high. “MCI stipulations for hospitals and college infrastructure are very stringent. We also need to woo faculty from clinical practice, which isn't easy ,“ said Dr Raj Bahadur, vice-chancellor, Baba Farid University of Health Sciences, Faridkot, which conducts centralised counselling for medical colleges in Punjab. Some heads also cited competition from other medical colleges as a reason for pushing up their fees.
Data collected by TOI from across the country suggests that studying medicine in the private sector could be most expensive in Tamil Nadu and cheapest in Gujarat and Karnataka. However, in many states, capitation fee is collected in cash over and above the hiked fees. For instance in Maharashtra, many private colleges are learnt to be taking Rs 40-60 lakh or Rs 70-75 lakh in the deemed universities. This makes it difficult to estimate the actual cost of private sector medical education.
That explains why activists are sceptical about capitation fees having been scuppered by NEET. “Even after the hiking of fees, a few colleges are still taking capitation fees in cash. But most are at least declaring higher fees instead of collecting cash under the table. To make it even more foolproof, the PAN number of the parents making the payment should be attached. And for every admission in the NRI quota, passport and citizenship details should be on record to be examined later in case of doubt of any fraud,“ said Dr Anand Rai, one of the whistleblowers in the Vyapam scam in Madhya Pradesh.
Members of state fee committees say they are aware of the climb in cost of medical education postNEET, but are helpless. “We can't do anything about it unless the public takes it up with the courts,“ said Dr C V Bhirmanandam, a member of the fee committee in TN.Committee members say they can only review tuition fees, not other charges.
“For medical colleges, these figures translate into business, but for parents and aspiring doctors they mark the end of their dream,“ said K Srinivasan, who was asked to pay Rs 40 lakh for his daughter's admission at a deemed university in Chennai.
(Put together by TOI's network of health reporters across India)
2021
Rema Nagarajan, March 7, 2021: The Times of India
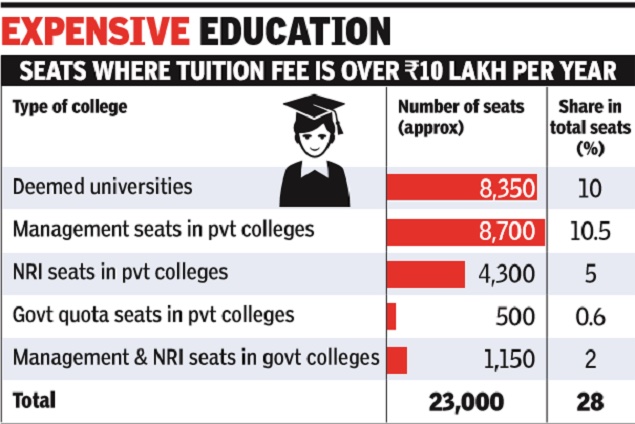
From: Rema Nagarajan, March 7, 2021: The Times of India
Quota for the rich? 28% of MBBS seats cost over Rs 10 lakh per year in tuition fees
About 28% of MBBS seats in India cost over Rs 10 lakh per annum in just tuition fees. The high fees effectively makes these seats a quota for the rich, one that is larger than those for the SC (15%), ST (7.5%) or OBC (27%). And that’s without taking into account the fact that this 28% is of total seats, while the caste-based reservations do not apply to all.
How did we get to this 28%? It’s based on a detailed analysis of fees for the MBBS course in over 530 MBBS colleges. About half the seats in private colleges, excluding deemed universities, are in the management quota or NRI quota. In the NRI quota, the average annual tuition fee is roughly Rs 25 lakh per annum. For the management quota, the average fees are around Rs 11 lakh though it varies from Rs 4 lakh in private colleges in West Bengal, which is uncommon, to Rs 18 lakh to Rs 20 lakh in states like Karnataka and Rajasthan. Besides the tuition fees, almost all colleges collect about Rs 2 lakh a year as charges for hostel, mess, exams, library and so on.
The most expensive seats are in the deemed universities. Over 8,500 seats in these universities constitute about 10% of all MBBS seats. Barely 3% or about 23,000 of the 7.7 lakh who qualified through the combined entrance exam, NEET, applied for these seats. The average annual tuition fees for NRI seats in these colleges are Rs 36 lakh, which is about Rs 1.6 crore for the entire course. The average fees for management seats in them are Rs 18 lakh.
TOI had reported earlier how the higher the fees, the poorer the average NEET score. The high fees leading to a virtual reservation for the rich has led to those with ranks even below 6 lakh in NEET getting admission, though there are only about 83,000 MBBS seats.
Even some government colleges, mostly in Gujarat (11 colleges) and Rajasthan (8 colleges) have management seats (1,350) and NRI seats (580) at an average Rs 18.5 lakh. The management quota seats in these government colleges range from Rs 7.3 lakh to Rs 18 lakh per annum in some of Gujarat’s municipal medical colleges in Gujarat. Others could also be as low as Rs 75,000 in Rajasthan to Rs 1 .3 lakh in Doon Medical College in Uttarakhand.
Most states governments have been pushing up fees in their medical colleges citing the high cost of medical education, though the money collected from increased fees is just a fraction of the budget. In Punjab, the cost of MBBS in government colleges went up from Rs 4.4 lakh to Rs 7.8 lakh, among the highest in the country. Fees in most government colleges in Maharashtra and Madhya Pradesh are about one lakh per year.
Incidentally, according to the latest expenditure survey done by the NSO in 2017-18, before the job loss of millions and economic devastation caused by the pandemic, the monthly expenditure of 80% of Indian families was less than Rs 10,500. Renowned economist Thomas Picketty had estimated that in 2015 about 5% of Indian adults earned over 63,000 a month or over 7.5 lakh a year. He estimated that just 1% (13.8 million) earned over 2 lakh. This is unlikely to have changed much since. What this means is that at best only 5% of families can afford the fees being charged for medical education in most institutions, even government ones.
Fifteen AIIMS accounting for about 1,100 seats offer the cheapest medical education, mostly charging Rs 1,628 or Rs 5,856 per annum. Centrally-funded institutions charge the least fees. West Bengal and Bihar offers the cheapest medical education in the country with the majority of colleges in the former charging Rs 9,000 as tuition fee and Rs 144 as hostel fees and the latter charging about Rs 6,000 as tuition fees and Rs 4,200-20,000 as hostel fees. Even among private colleges, West Bengal has among the lowest fees, mostly well below Rs 5 lakh for management seats and about Rs 15 lakh for NRI seats.
In 2016, the Parliamentary Standing Committee report on the functioning of the Medical Council of India (MCI) and medical education had strongly criticised “admission procedures which are primarily monetary based”. The committee recommended a common entrance test “to ensure that merit and not the ability to pay becomes the criterion for admission to medical colleges”. But with fees remaining unchecked, neither the new National Medical Commission nor the National Eligibility-cum-Entrance Test (NEET) has achieved this.
Deemed universities
MBBS admissions upheld for 2016: SC
SC upholds MBBS admissions by deemed univs, Sep 29 2016 : The Times of India
In a big relief to deemed universities in Maharashtra and Kerala, the Supreme Court on Wednesday refused to quash the admission process carried out by them for MBBS/ BDS courses on the basis of their own counselling in defiance of the government decision for centralised counselling.
Considering that admission for over 80% of the seats has been completed and classes have started in some deemed universities, a bench of Justice A K Sikri and Justice L Nageswara Rao upheld the admission but restrained them from holding further counselling for more intake.
“...will not disturb the admissions already made by the respondent universities... keeping in view that respondents are deemed universities,“ the bench said.
2018, 2019: limited competition for 8,000 seats
Rema Nagarajan, February 13, 2021: The Times of India
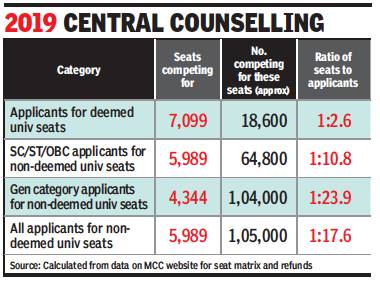
From: Rema Nagarajan, February 13, 2021: The Times of India
MBBS seats in deemed univs are still ‘reserved’ for the rich
High Fees Keep Competition Off 8,000 Seats
Though central counselling for MBBS seats in deemed universities was mandated in response to reports of seats being auctioned to those with the fattest wallets, seats in these universities continue to be an unofficial reserved quota for the rich.
Extremely high fees have ensured that those applying for 8,000 plus MBBS seats in 48 deemed universities face the least competition with just about three candidates vying for each seat in 2018 and less than four per seat in 2019, a TOI analysis of publicly available data shows. In comparison, for seats outside the deemed universities there were nearly 21 applicants per seat in 2018 and nearly 18 per seat in 2019. With fees ranging from Rs 20 lakh to Rs 25 lakh per annum, and even higher fees for NRI quota seats, of the nearly 8 lakh who qualified through NEET in 2019, less than 26,000 applied for 7,099 seats in deemed universities. Similarly, of the 7.1 lakh who qualified in 2018, less than 29,000 registered for 6,204 deemed university seats.
The Medical Counselling Committee (MCC) specifies that the quotas for OBC, SC, ST or PWD candidates do not apply in deemed universities. Thus, these seats effectively end up being reserved for the rich with wallets, not NEET scores, being the trump cards. To register for counselling for deemed universities seats, students have to pay Rs 2 lakh as security deposit compared to just Rs 10,000 for general candidates and Rs 5,000 for reserved category candidates applying for seats in the all-India quota (15% of seats in government medical colleges of almost all states) and seats in centrally-funded medical colleges.
Every year, a large number of seats that are not filled through centralised counselling are returned to the deemed universities, instead of the state counselling committee, to be filled at the institutional level. There have been numerous reports of seats going to the highest bidders in this process.
TOI calculated the number of candidates who registered for deemed university seats from the number of students refunded Rs 2 lakh at the end of the central counselling in 2018 and 2019. To this was added the total number of seats in deemed universities, since in the case of those who got a seat the security deposit was adjusted against college fees.
Similarly, the refund data also helped calculate how many general and reserved category candidates applied for the MCC counseling. Seats matrices for each year showed how many seats were open to those from general and reserved categories in the two years. This shows that the overall seat to candidate ratio for general category students was about 1:29 in 2018 and 1:24 in 2019. For reserved category students, it was 1:13 in 2018 and about 1:11 in 2019. Thus, in the centralised counseling, even reserved category students faced much tougher competition than those applying for deemed university seats.
High fees account for low quality intake
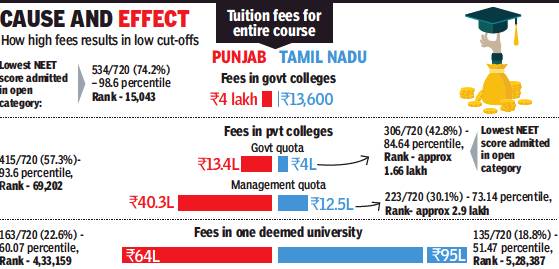
From: Rema Nagarajan, High fees in pvt med colleges account for low quality intake, April 21, 2018: The Times of India
With Up To ₹1Cr For Course, Only Rich Can Afford Medical Studies
There are only 60,000-odd MBBS seats in India, so how does someone ranked 4 lakh or more in NEET get admission even if he or she qualified? With all colleges having to go by the NEET ranking in admissions, this seems an impossible situation, but the high fees charged by most private colleges make it possible. That topples merit by forcing thousands of students with high scores to forego seats, allowing poor performers with money to get admission.
Take admissions to colleges in Punjab for instance — eight of them under the Baba Farid University of Health Sciences, three governmentrun and four private ones and a private university. The student with the highest NEET marks among those admitted into the private university had lower marks than the last student admitted to the open category in each of the government colleges.
In the private university, the fees for the MBBS course are Rs 64 lakh compared to just Rs 4 lakh in the government colleges.
While data for all states was not available, a similar pattern was evident in Tamil Nadu as well. In fact, even within private institutions, those who got into the government quota of private colleges had the best scores, while private universities saw candidates with much lower scores gaining admission. It’s no coincidence that the tution fees for the government quota in private colleges is fixed at Rs 4 lakh for the course compared to roughly a crore in the private universities.
To get a better sense of how exorbitant fees are lowering the standards of intake in medical colleges, consider this. If all 60,000-odd seats were in government colleges, where the fees are not prohibitive, the last rank to get in would have been at worst in the range of 80,000 even assuming that one-third of the top 60,000 ranks opted out for various reasons. The 80,000th rank in NEET 2017 had a percentile score of about 92.6 and marks of 399 out of 720, or about 55.4%.
Experts have suggested 1:3 as the ideal seats to eligible students ratio. That would have meant fixing the percentile cut-off so that about 1.8 lakh qualify.
In 2017, the cut-off would then have been 83.4 percentile, or roughly 295 out of 720 marks (41%).
The actual ratio achieved by the 50th percentile cut-off for general students and 40th percentile for reserved students was close to 1:10 with the lowest ranks even among general students getting as little as 131 out of 720 or 18%.
“Things have become much better with NEET, which stopped the completely unregulated MBBS admissions happening earlier. But to ensure that only meritorious students get in, the fees of these teaching shops that pass off as colleges have to be regulated so that students who perform poorly don’t use money power to defeat poor or middle class students who have scored much better.
“The government also needs to open more medical colleges,” said Dr Raj Bahadur, vice chancellor of Baba Farid University of Health Sciences.
Jawaharlal Shanmugam, who has filed a public interest petition in the Madras High Court seeking fee regulation in all medical colleges, pointed out that when NEET was introduced, many private colleges increased their tuition fees to offset the ‘loss’ of capitation fees.
“Thus they ensured that meritorious students without money would never get admission. The tuition fee is fixed arbitrarily to cater to only rich or super rich students. How can the government allow this when the Supreme Court had made NEET mandatory for even private colleges and deemed universities to ensure that medical admissions are meritbased?,”
Sale of private MBBS, MS, PG seats
The Times of India, January 30, 2016

Rema Nagarajan
You would never find advertisements for “confirmed admission“ to any IIT or AIIMS or one asking you to book a seat in advance in any of these premier institutes Neither are there advertise ments promising you selection for the civil services or place ment in an all-India service of your choice. Yet, the media is full of ads for MBBS seats in colleges across the country How, if the system is merit-based, can anyone promise “direct admission“? Behind this promise is a black market in medical seats in private colleges. With agents and college manage ments colluding to sell many of the 30,000-plus MBBS and over 9,600 postgraduation seats in private medical colleges, back-of-the-envelope calculations by TOI suggests hat about Rs 12,000 crore in hard cash changes hands in his black market every year.
Of the 422 medical colleges n India, 224 are private, accounting for 53% of MBBS seats.Many of these colleges are running with little or no facili ies, no patients and fake facul y. The going price for an MBBS seat could range from Rs 1 crore in colleges in Bangalore to Rs 25-35 lakh in some in UP . Seats in MD in radiology and dermatology cost up to Rs 3 crore. The prices could esca late or drop depending on how early you ap proach a college for a seat. If you book in advance, you could get a discount! Howev er, once the medical entrance results have been announced, the same seats at the private colleges will be sold for almost double the advance booking price. The sale of MBBS seats alone is worth almost Rs 9,000 crore annually .
Consortia of privately managed colleges and deemed universities that run medical colleges claim to conduct their own entrance examinations to take in students strictly on merit. However, in state after state, the exams have been exposed as a farce with students who pay money to buy seats being accommodated whether they appear for the exam or not and no matter what they score, while the so-called merit students are bumped off the list on various pretexts; with many even threatened and bullied into vacating seats.
While the 15% NRI quota seats are allowed to be allotted at the management's discretion in most states, in reality , even the management quota and a chunk of the so-called merit seats are sold off, bringing the proportion of seats sold to over 50%, the proportion rising to 80% or even 100% in some cases depending on how strict the regulation is in each state. The quota set aside for management varies from state to state. For instance, in MP and Maharashtra, the management quota is about 43%. This, plus the NRI quota brings the seats set aside to almost 60%.
With just 23,600 seats available for post graduate medical education, the demand for the same is very high. Thus, there is great demand for the 9,400plus seats in the private sector, including over 1,300 diploma seats. By a conservative estimate, about 40% of these seats also get sold. All told, the sale of post-graduate seats alone is estimated to be worth about Rs 2,900 crore. Add the highly valued seats for super-specialisation, about 370 in the private sector, of which again at least 40% is sold, and the postMBBS education black market figure crosses Rs 3,000 crore.Thus, along with the MBBS seat sale, the total amount comes to about Rs 12,000 crore.
The bulk of the money is paid in cash, leaving no trace of the transaction. And despite the advertisements giving the game away , the government has not cracked down on this black market or taken steps to arrest the rot in the medical education system.
Wide variation in fees

From: Rema Nagarajan, What explains huge variation in private medical college fees?, June 27, 2018: The Times of India
The average annual tuition fees for MBBS in private colleges varies from about Rs 5 lakh to Rs 25 lakh, with deemed universities typically charging the most. Data for the 2017 fees in about 210 private colleges given to the Medical Council of India shows only 25 averaged Rs 5 lakh or less and about half averaged under Rs 8 lakh.
“Are colleges charging Rs 5 lakh or less imparting inferior education? Or are those charging 20 lakh giving superior education? They are all following the MCI curriculum. How can there be such a huge difference?” asked Dr Vivek Korde of the Forum Against Commercialisation of Education. The difference can’t be explained by factors like higher costs in big cities.
In Pune, the average fees range from Rs 6 lakh to over 17 lakh, in Mumbai from Rs 7.7 lakh to Rs 25 lakh, and in Bangalore from Rs 4 lakh to 10 lakh. After the SC ruled that states can regulate medical college fees to curb commercialisation and promote merit, states constituted fee fixation committees. Colleges submit their expenses, on the basis of which the committees fix the fees.
Many claim higher expenses for extra amenities. However, Jawaharlal Shanmugham, the petitioner in a case against deemed universities in Tamil Nadu, pointed out that “luxurious facilities cannot be the criteria to fix exorbitant fees.” Dr Korde too said fees ought to be based only on expenses for facilities mandated by MCI. “Tomorrow, they could have a helipad, but they cannot charge students for it,” he added.
Many colleges allegedly inflate expenses through fake lists of teachers and staff. Last year, a Maharashtra college was in news for showing 250 teachers when students claimed there were just 41. Many deemed universities and their affiliated colleges have escaped the jurisdiction of the fee fixation committees. In Rajasthan, all private medical colleges are affiliated to deemed universities and their average fees range from roughly Rs 15 lakh to Rs 18 lakh.
In the eight deemed universities in Tamil Nadu, fees range from Rs 18.5 lakh to Rs 22.5 lakh. On Shanmugham’s petition, the Madras HC has asked the University Grants Commission to constitute a fee committee for deemed universities. Under the law, only nonprofit societies or charitable trusts could run medical colleges till the government in November 2016 permitted private companies to run them.
These trusts and societies are exempt from income tax on the grounds that they raise funds to provide affordable education for meritorious students. “If they charge the students for every paise spent on them, where is the charity?” asked Dr Korde, adding that it was a case of government inaction as most colleges were owned by politicians.
“Such high fees are beyond the reach of any common meritorious student. When the beneficiaries are rich students, these institutions do not perform any charitable activity,” stated Shanmugham.
Private medical colleges: controversy after MCI’s de-recognition order
2018: The case reaches the Supreme Court
Prasad, temples, judge’s words & 500% guarantee, January 16, 2018: The Times of India

From: Prasad, temples, judge’s words & 500% guarantee, January 16, 2018: The Times of India
MedEd Scam: Transcripts Of Discussions Recorded By CBI Suggest What Fixers Promised With Help From Contacts In Judiciary
‘Prasad’, ‘luggage’, ‘stuff’, ‘bahis’, ‘gamlas’: these mundane expressions, allegedly code for bribes, stand out in the conversations recorded by the CBI as part of its probe into the Lucknow Medical College scam, considered among the triggers of the troubles presently roiling the Supreme Court.
The transcripts, recorded by the Central Bureau of Investigation (CBI), of the discussions between retired Odisha high court judge I M Quddusi, who was jailed, alleged middleman Vishwanath Agarwala, and B P Yadav of the Prasad Education Trust have been cited to accuse them of seeking favours from the judiciary for the promoters of private medical colleges who were found to be lacking in infrastructure and, thus, asked to pause fresh admissions.
The recordings, in fact, suggest that the alleged fixers had promised a whole set of education entrepeneurs that they, with their contacts in the judiciary, will secure relief from Medical Council of India’s order to de-recognise courses and desist from admitting medical students. Two sitting judges of the Allahabad HC are already under the CBI scanner.
The accused persons also appeared to be cautious of stricter vigilance by the government over middlemen and ‘fixers’, with Agarwala saying that meeting with the concerned person was not possible because “tea seller’s government” is “watching everyone”.
But the businessman from Odisha offered “500% guarantee” that the work will be done. In one of the conversations, the transcript has Agarwala telling Quddusi that his point of contact — whom he refers to as “father” and “captain” — was “willing to do” whatever was required all over India. He will do it “100%”, he assures the retired high court judge.
At one point, Yadav is recorded telling Agarwala that he trusts the “judge’s words”. Agarwala again reminds Yadav that the issue will not be resolved if “prasad” is not given.
When contacted, CBI spokesperson Abhishek Dayal said that “the CBI will not confirm, deny or comment” on the PE or transcripts.
The suspeced references to judiciary with the businessman Agarwala boasting that he could get favourable orders from the “temple in Allahabad” as well as the “temple in Delhi”, resulted in a PIL being filed in the SC which was mentioned before a bench led by Justice Jasti Chelameswar, with the latter referring it to a five- judge bench. Chief Justice of India Dipak Misra, who has the final say in deciding which case goes to which bench, assigned the case, however, to a bench led by Justice A K Sikri.
Soon, an identical petition was again filed in the SC, which mentioned it before Justice Chelameswar and he, on this occasion, earmarked it for a five-judge bench.
The order was rescinded by a Constitution bench headed by CJI Misra, who asserted his prerogative as the ‘master of roster’. The four rebel judges — Justices Chelameswar, Ranjan Gogoi, Kurian Joseph and Madan Lokur — have charged that the CJI has used the power selectively to assign cases to “benches of preference”.
Apart from retired Justice Quddusi, accused of using his links with the judiciary, it is Agarwala, a businessman from Odisha, who emerges as an important figure in the manoeuvres to manage matters for “medical entrepreneurs” by manipulating judges. In fact, success of the moves seems to ride on the businessman who never failed to reassure Quddusi and the “ medical entreprenurs” that his contact will swing things for them.
In another conversation between Justice (retd) Quddusi and Agarwala, the businessman is heard asking Quddusi as to which “ temple” — the one in Allahabad or the one in Delhi” — the latter needed help from: expressions which CBI investigators suspect could be codes for wellregarded institutions.
CBI sources said that stuff, luggage, prasad etc are probably being used as code for bribe money. The transcripts reveal fierce negotiations over alleged bribe money with Yadav asking Agarwala to take ‘2 in advance’ and once the order comes out, he says, “We will get the admission; we will send 1 crore to the judge. Your place, Quddusi sir’s place, do it this way”.
Research
2005-14, neglected state
The Times of India, Apr 21 2016
Study reveals poor state of medical research
Rema Nagarjan
60% Of Institutes Don't Have A Single Publication In 10 Years, Only 4.3% Produced Over 100 A Year
A handful of institutes, a majority of them publi cly-funded, account for the bulk of research output from medical institutions in India. At the other extreme, nearly 60% of institutes did not have a single publication over a decade. Moreover, states that have the largest number of private medical colleges produce very little of research publication.
This was revealed in a study on the research output of all institutions in India during 2005-14 using Scopus, the largest database of peer-reviewed literature. The evaluation done by Dr Samiran Nundy, gastrointestinal surgeon and dean of Ganga Ram Institute of Postgraduate Medical Education and Research, along with two colleagues, looked at 579 institutes recog nised by the Medical Council of India (MCI) and the National Board of Examinations (NBE), which conducts the largest portfolio of examinations in medicine in India.
According to the study published in `Current Medicine Research and Practice', only 25 (4.3%) of the institutions produced more than 100 papers a year and these accounted for 40.3% of the country's total research output.Over 57% or 332 of the medical colleges did not have a single publication during this period while over 90% of NBE-affiliated colleges in Karnataka and Kerala had none.
The annual research output of the Massachusetts General Hospital and Mayo Clinic in the US was over 4,600 and 3,700 respectively.Even the most prolific research institution in India, AIIMS, published less than a third of these numbers. The top 10 medical institutes under MCI were AIIMS, Postgraduate Institute of Medical Education and Research in Chandigarh, Christian Medical College in Vellore, Sanjay Gandhi Postgraduate Institute of Medical Sciences in Lucknow, King George Med ical College in Lucknow, Kasturba Medical College in Manipal, Tata Memorial Centre in Mumbai, National Institute of Mental Health and Neurosciences in Bangalore, Institute of Medical Sciences of Banaras Hindu University , and Maulana Azad Medical Col lege in New Delhi. These accounted for 40.8% of the research output from the 579 medical institutions. The top 25 institutes under NBE, all private, contributed just 5.6% .
Overwhelming clinical burden leaving little time for academic activities is often cited as the reason for this state of affairs. “This is belied by the fact that the most prolific Indian publications come from institutions that also deal with the largest numbers of patients. This is also true of many of the world's great hospitals, which along with providing a high standard of patient care are also leaders in publication,“ observed the study .
It said lack of guidance and absence of role models among seniors, who themselves have published little, were major factors as was inadequate institutional support in the form of funds and infrastructure. However, the lack of incentives to do research and publish could be an even more important factor, since most faculty promotions in India are usually time-bound, based on seniority and influenced by political and bureaucratic `contacts', rather than on researching and publishing, the study noted.
The policy of increasing the number of doctors by liberally allowing the creation of new medical institutions, mainly through private funding and enhancing seats has not been an unqualified success with what is generally perceived as a fall in standards of medical education, “which has now become a business venture for many politicians and is accompanied by widespread corruption both in its entry and exit processes“, the study said, while calling for an overhaul of the medical education system.
Rules-/ eligibility- for admission to medical colleges
TN’s kinship and nativity requirements: 2018
Candidates seeking admission to MBBS and BDS courses in Tamil Nadu will have to produce at least eight of their parents’ documents, including birth certificates, nativity and income certificates and Aadhaar details, during counselling. They will also have to produce a document to establish their “relationship with the parents”.
A SSC notice on its website, signed by its secretary Dr G Selvarajan, has said students looking to take admission in government and self-financing colleges must produce original certificates and documents.
They have been instructed to bring 10 documents, including NEET hall ticket, Class X and XII marksheets, certificate to prove they’ve studied in one or more schools in TN between Class VI and XII, community certificate, first graduate certificate and ration card/passport besides proof of relationship with the parents. Dr Selvarajan said documents of parents were required only if the candidate hadn’t studied from Class VI to XII in TN.
Selection (by means other than merit)
Check on your doc before a check-up
Rema Nagarajan TIMES INSIGHT GROUP
The Times of India 2013/07/21
With the Supreme Court striking down the common entrance test for medical colleges, patients face the growing prospect of being treated by doctors whose merit may not have been adequately tested.
With the creation of more and more private medical colleges, many experts fear students will increasingly buy their way into becoming doctors from such institutes, many of which are notorious for their lack of teaching and training infrastructure.
These students do not have to face any centralized external exam to get their degrees. Exams are conducted internally, most often by private or socalled deemed universities that run medical colleges.
1 in 5 doctors bought a seat in medical school
Back-of-the-envelope calculations show that about one out of every five doctors passing out each year, or around 8,000, could be those who effectively bought seats in medical colleges. The consequences for public health are fairly obvious.
The ‘management quota’
Going by what is allowed under existing rules, nearly 15% of seats in private medical colleges across the country are in what is called the management quota. This term is widely recognized as a euphemism for seats available to those who can pay for the privilege. Estimates of exactly how much a seat costs vary, but the amount could be Rs 30-90 lakh, depending on the location of the college, its reputation and the timing of the booking.
Currently, over 25,000 seats for medical graduate admission are in private medical colleges compared to just over 20,000 in government colleges. The 15% kept aside for the management quota amounts to 3,750 seats. However, the actual quota is usually way higher than 15%. It could go up to a third of the seats, or in some cases, even over half the seats in a private college. Even a conservative third of the seats being sold as management quota would mean that over 8,000 seats are being sold.
Proxy students take the examinations
In a scam uncovered in Bangalore, it was found that qualified people were employed to write the entrance exams and such proxy students after getting allotment of seats through counselling would surrender the seat leaving it available to the management to allot at its discretion, which it would do in return for as much as Rs 75 lakh to Rs 90 lakh. This, according to several admission agents, is still a common practice.
All the money for booking the seat is collected in black and seats are booked as early as December of the year before the year of admission, way before any entrance exam. Of course, they stipulate that the admission is on the condition that the student gets 50% in class XII.
“With increasing variation in the quality of medical education and the unearthing of seat selling scams, we might need an exam for all medical graduates to test and certify their level of knowledge before they are to allowed to practice — something similar to the exam that foreign medical graduates have to clear to be allowed to practice here. Such a proposal had been made before,” said Dr Bipin Batra, executive director of the National Board of Examinations, which conducts the National Eligibility cum-Entrance Test for postgraduate medical education and the examination for FMGs. On grounds of bridging the shortage of doctors, the Medical Council of India has been approving the creation of more medical colleges and expanding the number of seats.
’Seats’ in medical colleges (number)
From pre-independence to 2019
Rema Nagarajan, June 14, 2019: The Times of India

From: Rema Nagarajan, June 14, 2019: The Times of India
Biggest-ever addition to govt MBBS seats in 1 yr: 2,750 in 25 new colleges
The academic year 2019-20 will see the biggest addition of medical seats in government colleges in a single year, with 2,750 seats in 25 new government medical colleges having been created. Though the government has been on a significant expansion spree in medical seats since 2012 after decades of sluggish growth, the process has accelerated in the last two years with new colleges being created and existing ones also increasing seats with the help of central funding.
The biggest stumbling block to the expansion of medical education has been inadequate availability of faculty, a problem that persists despite the government repeatedly diluting faculty requirements. With the private sector too adding 10 new colleges in 2019, accounting for 1,500 seats, the minimum faculty requirement for the 35 new colleges is well over 3,000 — over 600 professors, 1,000 associate professors and almost 1,500 assistant professors. With even existing medical colleges struggling to find faculty, medical educationists are concerned that this could lead to more unethical practices like ghost faculty and poaching of faculty from established government colleges.
Former Union health secretary Sujatha Rao tweeted: “Where do they get the faculty from? How do they ensure quality of training? Choice seems to be between having a shortage of doctors and illtrained doctors.”
Dr Vinod Paul, chairman of the Medical Council of India’s board of governors and member of Niti Aayog, told TOI that measures such as increasing the retirement age and getting those retired from the armed forces to come back to teaching had already been initiated to address the issue.
Are there enough faculty for expansion of med colleges?
In 2018, the government added 18 colleges and the private sector five. The minimum faculty requirement for these would be 2,000. In 2017, 13 colleges were opened requiring over 1,100 faculty. In 2016, 30 colleges were opened. The faculty requirement for these would be about 3,000. Thus from 2016, over 100 colleges were opened requiring over 9,000 teachers. The question is whether there is adequate faculty available for this level of expansion.
With the expansion in 2019, there are now 70,978 MBBS seats in 529 colleges in India. Of this, 269 colleges accounting for 35,688 seats are government-run, while the remaining 260 colleges accounting for 35,290 seats are in the private sector.
While new government colleges typically get just 100 seats, 94 out of 108 private colleges opened since 2010 got 150 seats each. In the same period, only 30 of 123 new government colleges got 150 seats. This tendency to grant private colleges more seats is despite that since 2010, 15 private colleges were either barred from taking students or shut down, in most cases because of inadequate patient load and faculty. While it makes sense to give fewer seats to an institution just being set-up, why the same logic not apply to private colleges despite having a bigger problem in getting patients to a new set-up?
Super- specialty courses
2017: 1/3 seats are vacant
After close to 550 super-specialty medical seats in the country remained vacant this year in the firstever centralized admission process through NEET, Union ministry of health and family welfare is planning stringent measures to prevent vacancies and ensure meritorious students are not left without seats.
For one, doctors may hen ceforth be barred from the process for a year or two if they do not accept seats allotted in a given year. Also, candidates may have to pay upfront a higher fee (up to Rs 2 lakh) for NEET counselling as deposit and it will be transferred to the college where they are admitted. But the money will be forfeited if they fail to continue with the course.
Of 1,907 superspecialty seats available this year, 550 remained vacant after two admission rounds. Over 200 remained vacant in state-run colleges. Two court cases and a stay for a few days delayed the process. As September 14 was the last day for admission, government could not hold a third round. Before this, super-specialty seats were filled by states or individual institutes.
“Many candidates selected seats but did not join. These seats remained blocked. Vacancies were known after completion of rounds,“ said an official from the ministry. While the ministry plans tough measures, nothing is finalised yet.“It is unfortunate seats were available in government colleges but meritorious students were unable to take it,“ said the official.
The reason students backed out is states like Tamil Nadu, Telangana and Andhra impose mandatory rural service for 5-10 years and set a bond of Rs 2 crore if they fail to fulfil it, said the official. “Most doctors finish MD at age of 30-35 and seek admission to superspecialty when they are in their late 30s or early 40s. They did not want to do a rural stint of 10 years at this stage,“ said the official. For admission to superspecialty courses at all-India level, NEET Superspecialty , was held. Courses on offer included doctor of medicine (DM) in different branches and other Master of Surgery (M Ch) courses.
Tests for admission to medical colleges
National Eligibility cum Entrance Test (NEET)
Binding on private colleges; states to fix eligibility criteria
The Times of India, May 06 2016
AmitAnand Choudhary
No MBBS entrance test by pvt colleges: SC
The Supreme Court ruled out separate entrance tests this year by private medical colleges for admission to MBBSBDS courses but said it would consider the states' plea against implementation of NEET this year on the ground that students were caught unprepared.
The court had on April 28, 2016 made performance in the National Eligibility cum Entrance Test (NEET) the sole criteria for getting admission to government and private medical colleges and said the May 1 AIPMT would be considered as first phase of NEET. But this created confusion as by that time several states had already conducted entrance tests.
With a large number of private medical colleges and governments moving the SC seeking clarifications and modification of the April 28 order, a bench of Justices A R Dave, Shiva Kirti Singh and Adarsh K Goel on Thursday said, “There is no question of permitting examinations by private colleges.“ Tests conducted by states continue to be under the court's consideration.
The court asked the Centre, CBSE and Medical Council of India to suggest ways to accommodate states, which pleaded that they had a statutory obligation to conduct entrance examination for medical colleges run by them.They also said students, particularly from rural areas, would not be able to compete for NEET as they had prepared for state examinations held in vernacular medium. Various states, including J&K, Gujarat, Karnataka, Tamil Nadu, UP, Maharashtra and Andhra Pradesh told the bench that once they had conducted the entrance tests under the law, NEET could not have been imposed on them. Senior advocate Gopal Subramaniam and lawyer Sunil Fernandes, appearing for J&K, said the state enjoyed special status and it had been allowed to hold separate entrance test.
The bench, however, said states were free to fix eligibil ity criteria for admitting students. The Centre, which had earlier supported the states, batted for NEET and told the bench that a common entrance test did not violate state laws. “ Who is to be admitted, what should be the eligibility criteria and reservation criteria are to be decided by the states,“ solicitor general Ranjit Kumar said.
He, however, suggested that many students, who had applied for AIPMT but did not appear, should be allowed to appear in the second phase. The SG also suggested holding a composite test on July 24 .
CBSE counsel Pinky Anand said it was difficult to hold a composite test as the number of students would be huge. Around 6.5 lakh students had taken the May 1 NEET. The court adjourned hearing in the case to Friday .
3 attempts; age limit 25 (unreserved)/ 2017
Hemali Chhapia, Jan 25, 2017: The Times of India
Medical aspirants across India can now only take three shots at the National Eligibility cum Entrance Test (NEET), a cap introduced to discourage the thousands who keep trying their luck at the examination. Also, candidates must fulfil a new age criterion if they wish to sit for the medical and dental exam.
The decision was taken at a University Grants Commission (UGC) meeting on Tuesday in Delhi. The minimum age to appear for NEET is 17 years. The maximum age for open category students is 25 years, and 30 years for the reserved category . To date, there has never been a maximum age defined to take NEET, nor has there been a limit on the number of attempts. “This is a good decision,“ said Dr Pravin Shingare, director at the Maharashtra directorate of medical education and research (DMER).
“There are some students who keep taking the test, and when they don't make the cut, join a BSc college and keep taking the medical entrance test,“ he added. In fact, the rule would also bar the facul ty of coaching classes who keep on attempting the test to understand its altering pattern. The NEET information brochures contain this information and will be distributed soon. “We often find that coaching classes field candidates and sometimes that leads to fraud and cheating,“ said an expert. This cap on age and attempts will force candidates to focus on the field where their capability and passion lie, said medical college principals.
Two years ago, it may be recalled, the All India Pre Medical Test had to be conducted again as it was revealed that 90 answers had been transmitted to the candidates during the ex amination, for a fee of Rs 15 to 20 lakh. The AIPMT-2015 scandal had at least 45 beneficiaries who were supplied with special vests fitted with SIM cards and a bluetooth device, among other equipment, to facilitate the transmission of answers.
While all-India data is unavailable, in Maharashtra, the number of older candidates competing with 17-yearold aspirants has been rising with each passing year. About 12,000 repeat aspirants took the CET in 2007, while in 2008, the number grew to 13,568. According to data collected from the DMER, the oldest candidate was 38 years old and at least another 100 aspirants were in their early 30s.
Seats: 2016> 2017

From: Rema Nagarajan, April 15, 2018: The Times of India
Percentile Drives Cut-Offs To Absurd Low
With just 5% marks in physics, less than 10% in chemistry, and 20-odd per cent in the biology section of the National Eligibility-cum-Entrance Test (NEET), candidates have got admission to medical colleges in the past two years. This was made possible by the “percentile” system under NEET that was supposed to keep non-meritorious students out.
Before NEET was made mandatory in 2016, the cutoffs for admission were 50% marks for the general category, and 40% for the reserved categories. From the 2016 admission year, these were changed to 50th and 40th percentile, respectively, opening the doors to candidates with just 18-20% marks in the NEET aggregate.
Here’s how it happened. In 2015, you needed 50% marks for admission in the general category, so you would have had to score at least 360 out of 720 marks. But in 2016 you only needed to be in the 50th percentile, which meant scoring 145 out of 720, or barely 20%.
2019/ Candidates with very poor marks are admitted
Rema Nagarajan, June 15, 2019: The Times of India

From: Rema Nagarajan, June 15, 2019: The Times of India
The qualifying percentile for NEET being kept as low as 50th percentile has meant that about 50 students who scored single digit marks in physics or chemistry out of 180 in the entrance exam got admission in medical colleges in Punjab alone in 2018. Of these, seven had zero marks out of 180 in one of these subjects and another 10 had negative marks. This raises questions about the rationale of testing students in physics and chemistry if after getting such abysmal scores they still managed to get into MBBS.
Over 85% of those who got admission with single digit marks in at least one subject were admitted to private colleges. As TOI’s analysis last year of the 2017 MBBS admissions showed, colleges charging the highest fees typically had the poorest average NEET scores for those they admitted. In Punjab’s case in 2018, Adesh Medical College, which charges about Rs 68 lakh for the full MBBS course, accounted for more than half the students admitted with single digit, zero or negative marks in physics or chemistry. The college does not come under fee regulation since it is affiliated to a group-owned university. Adesh also had the lowest average NEET score for MBBS admissions among all the medical colleges in the state.
While this analysis is for Punjab alone, the 2017 experience suggests the pattern would be the same in other states too and much worse in many. However, since neither the Medical Counselling Committee nor the Medical Council of India make the NEET score, rank, percentile and individual subject marks scored by students admitted each year public, the farce of claiming that NEET has ensured that all admissions are ‘meritbased’ continues.
In most colleges with high fees, despite students with high scores being eligible for admission, they are forced to drop out as they cannot afford the fees. With over 7 lakh students qualifying for about 65,000 seats (a little over 70,000 this year), there were enough candidates with poor scores but deep pockets who could take the place of those with high scores who could not afford the hefty fees.
Just how bad is a zero or negative score in a subject? The NEET exam consists of 45 objective type questions each in physics and chemistry and 90 in biology. Each question has four options. A correct answer gets four marks but a wrong answer leads to one negative mark. Elementary mathematics shows that a person marking the answers at random is likely to end up with about onefourth of the answers right and the other three-fourths wrong. That would mean a score of about 10 out of 180 (11x4 for the right answers minus 34 for the wrong ones). So, someone getting less than 10 out of 180 is doing worse than an illiterate person would do if asked to randomly pick answers. Yet, such a candidate is not just qualifying through NEET but getting into medical college. Despite these anomalies being pointed out last year, the government has refused to fix individual subject cut-offs.
SC: Only one test
The Times of India, Apr 28 2016
AmitAnand Choudhary
Only 1 test for medical admission from this session itself, rules SC
Even as lakhs of students prepare for entrance examinations conducted by state governments and private colleges for admission into medical colleges, the Supreme Court insisted that multiple tests must give way to the National Eligibility Entrance Test (NEET) for the 2016-17 session.
The test season was to kick off from May 1when CBSE will conduct All India Pre-Medical and Pre-Dental Entrance Test.It will be followed by Maharashtra CET on May 5 and the test conducted by private medical colleges of Karnataka on May 8. Around five other entrance tests are scheduled for the next month, including the one conducted by AIIMS.
NEET, which was declared illegal and unconstitutional by SC in 2013, was restored on April 11after a five-judge Constitution bench recalled the earlier verdict and allowed the Centre and the Medical Council of India (MCI) to implement the common entrance test till the court decides afresh on its validity.
Despite the revival of NE ET, the authorities failed to implement it, forcing NGO Sankalp Charitable Trust to approach SC for enforcing the mechanism for a common test for admission in MBBS, BDS and PG courses in all colleges. New Delhi: The Supreme Court on Wednesday told the government that multiple medical entrance tests must give way to the National Eligibility Entrance Test (NEET) from the 2016-17 session itself.
Advocate Amit Kumar, appearing for the petitioner NGO Sankalp Charitable Trust, told a SC bench of Justices A R Dave, Shiva Kirti Singh and A K Goel that the Centre, MCI and CBSE were dilly-dallying in implementing the court's order on implementing the National Eligibility Entrance Test (NEET), compelling students to appear in as many as 90 entrance exams across the country for admission.
“A student seeking admission in a medical college has to shell out lakhs of rupees in taking an examination and most of the tests are not conducted in a fair manner. There is no impediment in way of implementing NEET after the Constitution bench verdict and the Centre should be directed to enforce the order in association with MCI and CBSE,“ Kumar told the bench.
The bench agreed with his contention and said NEET must be implemented from the coming academic session itself. It directed the Centre, MCI and CBSE to sit together and frame a time-schedule for conducting NEET. It directed them to place before it by Thursday a dateline for the common entrance test. The counsel appearing for the government, MCI and CBSE told the bench that there were “willing and committed“ to hold NEET for 2016-17 and agreed to place the proposed time-schedule on Thursday .
The Constitution bench had said that the controversial judgement of July 2013 by which NEET was quashed needed reconsideration as the “majority verdict“ delivered by then CJI Altamas Kabir did not take into “consideration some binding precedents and more particularly , we find that there was no discussion among the members of the bench before pronouncement of the judgement“.
Lakhs of students appear for various medical entrance examinations in more than 400 colleges and there are more than 52,000 seats available for MBBS courses. After the scrapping of NEET, states and private colleges have been conducting exams separately for the last three years.
Failing CET, but getting govt medical college
The Times of India, Apr 07 2016
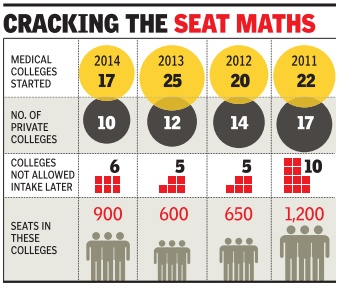
Rema Nagarajan
Didn't get admission in to the best government medical college in yo ur state? Not even the bottom-rung ones? Don't worry .Your best bet may be to buy a seat in the worst private medical college in the state and pray it doesn't get permission to admit students in the coming years. If that happens, you can go to court and the state government may be ordered to accommodate you in the very colleges you could not get into.
That may sound like a bizarre strategy , but it is exact zarre strategy, but it is exactly what has been happening in many states. Several private colleges have failed to get permission to admit students after the first, second or third batch. Then the regular pattern of petitioning courts and getting accommodated in government colleges plays out.
An analysis of data on student intake allowed per college, available from 2011, showed that around 42 colleges across the country , almost all private, were barred from admitting students for a year or more in this period, in some cases since the first batch was taken in.
How can a medical colle ge given permission, and allowed to admit students one year, be found deficient subsequently and barred from intake? This is because the Medical Council of India (MCI) allows any trust, society or company to start a medical college, even if it doesn't have the required infrastructure and faculty. Medical Council of India rules need a new medical colle ge to show it has good enough infrastructure for first year MBBS students' requirements and an undertaking that the rest will be put in place.
MCI assessors inspect a new college every year for five years and issue permission for each year.When they fail to stick to their commitments, the regulator cracks down and doesn't allow further intake. This often works to the advantage students, although after a legal battle.
“College managements constantly hustle the authorities to give them permission to start taking in students even when there is almost no infrastructure.With political connections (most trusts are either run by politicians or their family members), they manage to get permission,“ said a medical college professor.
Every year, MCI decides that several colleges, which had received conditional approval and admitted students, are “not approved permitted for intake“ as the institutions do not have infrastructure. Following this, dozens of cases are filed in high courts and the Supreme Court by the management of these colleges and by students or their parents. In 2015, 27 colleges with 3,650 seats were not allowed to admit students.
Of the 10 private medical colleges started in 2014, six (accounting for 900 seats) were not allowed to admit students in 2015. So, what happens to the 900 students admitted in 2014 after paying lakhs as capitation fee? “When denied permission, college managements tell students and their parents to go to court and seek relief if they don't want their investment to go to waste,“ explained a lawyer.
Getting 0 or less in NEET papers, but admitted to MBBS/ 2017
Rema Nagarajan, Some MBBS students got 0 or less in NEET papers, July 16, 2018: The Times of India

From: Rema Nagarajan, Some MBBS students got 0 or less in NEET papers, July 16, 2018: The Times of India
No Cut-Offs For Individual Subjects
With no cut-off for individual subjects –physics, chemistry and biology—in the NEET entrance exam, at least 400 students with single-digit marks in physics and chemistry and 110 students with zero or negative marks in them have been admitted for MBBS in 2017, mostly in private colleges. This raises a question. If getting zero in these subjects doesn’t make a person ineligible for admission, why bother to test in that subject at all?
Interestingly, the original notification to adopt a common entrance examination had stipulated that students should score at least 50% in individual subjects. However, the subsequent notification, which brought in the percentile system, dropped the stipulation on marks in individual subjects.TOI analysed the subject marks of 1,990 students who got admitted to MBBS with NEET scores of less than 150 out of 720 in 2017. We found 530 with single-digit marks, zero or less in physics or chemistry or even both.
There would be many more such examples among those admitted in MBBS courses with aggregate marks above 150.
Out of these 530, 507 were in private medical colleges. The average tuition fees paid by them (not including hostel, mess, library and other miscellaneous charges) were about Rs 17 lakh per annum showing how rich students with abysmal NEET marks have effectively been able to buy their way into medical colleges. NEET, promising a merit-based selection, was meant to prevent exactly this. About half of these students are in deemed universities which would be free to conduct their own final MBBS examination.
Once cleared, these exams would allow their students to register and practise as doctors. NEET was first mooted in a December 2010 gazette notification of the Medical Council of India (MCI), then administered by the government appointed Board of Governors. The notification specified that eligibility for the MBBS course would be by obtaining at least 50% of marks (or 40% in the case of reserved categories) in “each paper of NEET”.
However, a subsequent MCI notification in February 2012 not only changed the eligibility criteria from 50% and 40% to 50th and 40th percentile, but also did away with minimum marks in each paper. When the Supreme Court in 2016 reversed its earlier order to pave the way for NEET to be implemented, it effectively revived this notification. Dr KK Talwar who headed the BoG in 2012 explained to TOI that faced with stiff resistance to NEET from state governments, the focus then was on finding a way to get NEET accepted. “If the NEET results over the years show that the percentile cut off is too low, or that minimum marks need to be fixed, there is nothing stopping the MCI from making necessary amendments,” said Dr Talwar.
SC: Age no bar on upper age limit
AmitAnand Choudhary, Age no bar to become a doctor: SC, April 1, 2017: The Times of India
25-Yr Age Cap For Taking NEET Erased
All aspiring medical students can now appear for NEET in 2017 irrespective of age as the Supreme Court removed the age cap of 25 years fixed by CBSE for taking the entrance examination for MBBS courses.
A bench of Justices Dipak Misra and A M Khanwilkar said the decision taken by CBSE to fix upper age limit on the administrative instruction of Medical Council of India seemed wrong and students should not be barred from appearing in the entrance examination.
The court directed CBSE to open a window till April 5 for those above 25 years to apply for the National Eligibility Entrance Test (NEET) which is scheduled for May 7. The last date for filling up forms was March 1.
The bench agreed with the submission of the aggrieved students who contended that the decision taken by the Board was illegal and unconstitutional as there were no rules or regulations for fixing upper age limit for medical entrance examination. Senior advocates Amrendra Sharan and Indu Mal hotra, appearing for the students, told the bench that about 20,000 candidates got affected due to age restrictions and pleaded the court to allow them to appear for NEET.
“As we, prima facie, find, such an age limit could not have been determined by way of a notice on the basis of the instructions issued by the Medical Council of India. It is appropriate to direct that all the desirous candidates will be allowed to fill up the forms on the online portal of CBSE on or before April 5. Any form submitted beyond April 5 shall not be accepted,“ the bench said. The court asked CBSE to take steps to make arrangements to allow the affected students to appear for the entrance test and provide additional centres to accommodate them.
Centre's omission of Urdu for NEET is bias: Petitioner
A students' organisation told the SC on Friday that the Centre had deliberately left Urdu as a medium to take NEET as the government is “prejudiced and biased“ against Muslims.
Appearing before a bench of Justices Kurian Joseph and R Banumathi, Delhi-based Student Islamic Organisation's counsel Ravindra S Garia contended that the Centre's decision to allow students to take the exam in one of the ten languages -Hindi, English, Gujarati, Marathi, Odiya, Bengali, Tamil, Telegu, Kannada and Assamese -but not in Urdu showed its bias against the minority community .
“It is deliberate and intentional on the part of the health ministry to not include Urdu as a medium for NEET exam because of the discriminatory perception of the government functionaries of viewing the language not as a part of cultural heritage and composite culture of India, but as a language associated with Muslims,“ the organisation said in its affidavit.
Taking strong exception to the allegations, Solicitor general Ranjit Kumar said it was a very serious charge against government as the students' body had termed the Centre as “communal“ and sought the court's permission to file response. The court granted the Centre one week's time to file response .
Women studying medicine
1991-2015
The Times of India Jan 10 2016

More women studying medicine, but your doctor still likely to be a man
Rema Nagarajan
The first Indian woman physician, Anandibai Joshi, graduated in 1886. About 125 years later, Indian women started to outnumber men in admissions to medical colleges and the trend continues to grow stronger by the year: over the last five years, India has produced over 4,500 more female doctors than male ones.
In India, women constituted 51% of the students joining medical colleges, cornering 23,522 seats in 2014-15 compared to 22,934 men. This increase is in keeping with the worldwide trend. In fact, in the neighbourhood, Pakistan and Bangladesh have much higher proportions of women in medical colleges, 70% and 60% respectively.
However, there is a serious shortage of female doctors in India. According to a paper titled Human Resources for Health in India, published in 2011 in the medical journal Lancet, only 17% of all allopathic doctors and 6% of those in rural areas are women. This is less than one female allopathic doctor per 10,000 population in rural areas (0.5), whereas the ratio is 6.5 in urban areas. The number of female doctors per 10,000 population ranges from 7.5 in Chandigarh to 0.26 in Bihar.
According to a paper on women in medicine published in the journal, Indian Anthropologist, by sociologist Dr MitaBhadra, the gender gap persists at the post-graduation and doctoral levels -the percentage of female doctors here is around onethird of male doctors. She also observed that positions of leadership in academics and administration are still mostly occupied by men.
In Pakistan, though 70% of medical students were women, only 23% of registered doctors were female because a large number of those who graduated never took to practising. Bangladesh produced 3,164 female doctors and just 2,383 male doctors in 2013. The trend of more women joining the medical profession is welcomed as female doctors are seen as more committed and caring.
A paper on women in medicine published by Dr 46.5 Rakesh Chadda and Dr MamtaSood of the psychiatry department 37.3 of AIIMS in the Indian Journal of Gender Studies noted that medicine has been a 38 male-dominated profession because it demands long working hours that are disadvantageous to women who, even today , struggle to juggle career and family responsibilities.
The paper noted that though women were earlier largely restricted to fields like obstetrics, gynaecology and paediatrics, this was changing. “There has always been a preponderance of women in preclinical subjects like anatomy , physiology and biochemistry and paraclinical subjects like pharmacology , pathology and microbiology rights from the '70s. However, when a department is headed by a woman, the percentage of women faculty in the department goes up. In departments headed by women the women faculty was 49% as compared to just 19% in those headed by men,“ says Dr Chadda, giving the example of the neurology depart ment in AIIMS, which saw a lot of woman faculty joining when the HOD was a woman. “It is probably because the head of the department becomes a role model and more women are encouraged to join,“ said Dr Chadda.
There are skews within the medical profession in most parts of the world with some medical specialties, such as surgery and other disciplines requiring emergency duty with irregular hours, being male-dominated. Even in the UK, though women account for over 56% of those opting for medical education, 44% are pediatricians, 49% are in public health and only 8% are surgeons, according to a Royal College of Physicians report.
Among the OECD countries, in 10, predominantly from the erstwhile Eastern Bloc, the proportion of female physicians is more than 50%, ranging from a high 73.8% in Estonia to 50.2% in Spain. In two non-OECD countries for which the OECD had data, Latvia and Lithuania, females accounted for over 74% and 70% of physicians. In contrast, only one in five doctors in Japan and Korea were women. In the US, it is one in three.
2015-18/ Fewer girls; NEET to blame
Hemali Chhapia, July 31, 2018: The Times of India’'

From: Hemali Chhapia, July 31, 2018: The Times of India
For the past many years, girls in Maharashtra used to outnumber boys in making the cut to join medical schools. Neither the intensity nor the length of the course deterred these young, determined women. This year though, the trend has reversed— more boys will sign up for MBBS in colleges across the state. Directorate of medical education and research data shows that 1,448 young men will make it to public medical schools against 1,123 young women in 2018. Compare these to last year’s figures of 1,182 boys and 1,488 girls.
Experts attribute the turnaround to NEET, the all-India exam that involves a more rigorous preparation than the earlier MH-CET. Fewer families let girls travel away from home and sign up at coaching hubs in Hyderabad and Kota for intensive NEET coaching.
Intensive NEET coaching might be working in favour of boys: Med prof
Some girls do not get the push required for the two-year preparation after Class X. As NEET is based on NCERT curriculum, unlike the state’s CET, intensive coaching may be working in favour of boys,” said a medical school professor. NEET (National Eligibility and Entrance Test) was introduced in May 2014 as a pan-India examination but it was scrapped in September the same year after receiving flak from students. States then began conducting their own CETs, based on the local school board syllabus. In April 2016, the Supreme Court reintroduced NEET, scrapping all state CETs to make NEET the single-window entrance exam for admissions to all medical and dental institutes in the country. “Now, with NEET, the trend in Maharashtra has turned around. We will see more boys join the MBBS course this year as compared to what we saw in the previous years,” said Pravin Shingare, head, state DMER.
Some fear this trend may hold true across the country. While the success rate of girls in NEET is better than that of boys nationally, higher ranks elude them. Of the total 13.3 lakh students who registered for the test, 56% were girls. The success rate of girls is also around the same.
This year, there were a mere 14 girls in the Top 50 NEET rankers. When Maharashtra conducted its own CET, girls performed better. In 2008, 49 girls were in the Top 100 ranks in the state entrance merit list. The numbers gradually dropped to the 30s, and this year to 28.
The 2018 trend has turned around to the time when the state saw its first woman doctor, Anandibai Gopal, graduate in 1877.
For years, most girls shied away from the medical profession—perhaps because of the length of the course or gruelling work hours—with graduating batches till almost the mid-1980s producing more male doctors. Soon, the skewed gender ratio started turning around though.
The 2011 data shows that 1,091 girls joined the course against 967 boys. For long, in almost all health sciences programmes, more girls took admission in courses such as nursing, dentistry and physiotherapy.
When Dr Partha Roy entered a medical school in 1974, 10% of the students were girls. The trend reversed in 1980s and had continued since.
When Dr Rajeev Chhabra joined Grant Medical College in 1981, there were 60% girls in his class. “This was when there was no coaching. Girls did well in school and high school, and many went on to qualify for medicine. Today, you will see coaching for NEET has altered the gender ratio. Look closer and there are many more boys in the reserved categories,” said Chhabra.
Whether more girls return to the bastion that they once ruled, only time will tell.
Viruses
Covid-19
2020: India 5th country to isolate virus
Will Help In Developing Drugs, Vaccines, Rapid Diagnostic Test Kits: ICMR '
India has become the fifth country to successfully isolate a strain of the novel coronavirus. China, Japan, Thailand and the US did it before.
Simply put, it means that scientists have been able to obtain a pure sample of the virus that has been contained outside the human body.
The scientific success is important because it will help in developing drugs, vaccines and rapid diagnostic test kits, the director general of Indian Council of Medical Research (ICMR), Dr Balram Bhargava, said.
He added that the isolation of the novel coronavirus, the agent responsible for the ongoing outbreak of Covid-19, wasn’t easy as India had fewer positive cases when they started the project. “Total 21 throat swab and nasal swab samples were examined for this purpose. Of that, 11 tested positive and eight strains could be isolated from among them. They are 99.98% identical with the strain of the virus that led to outbreaks in Wuhan in China,” said Dr R R Gangakhedkar, chief epidemiologist at ICMR. He added that now scientists can test whether a drug will work against the virus or not to develop rapid diagnostic kits.
The isolation of this virus will also help in understanding the biology and evolution of the novel coronavirus, say ICMR experts. Till date, there is no cure for Covid-19. Also, there is no preventive vaccination.
Anti-HIV drugs lopinavir and ritonavir have been tried on some Covid-19 patients, including the Italian national admitted at Sawai Man Singh hospital in Jaipur, with promising results. But the scientists said it is too early to conclude the efficacy. Most patients are only receiving symptomatic treatment, they added.
Recently, in a draft report made public by the World Health Organisation (WHO), the experts claimed that Remdesivir, a drug developed for use against ebola, which caused major outbreaks in remote villages in Central Africa in 2014, is most promising for treating Covid-19.
This is because the in-vitro (tests performed in test tube) and in-vivo (tests performed in living organism) data for the drug is available for coronaviruses. “Further, studies in mice using Remdesivir showed superior efficacy over Kaletra+IFNbeta,” the draft report said.
The report added that a clinical trial is being planned in China to evaluate the safety and efficacy of the drug in association with optimised standard of care, as the next step. Remdesivir slows the infection of healthy cells by blocking viral replication.
The WHO expert also reviewed drugs used in HIV treatment — lopinavir and ritonavir — either alone or in combination with IFNbeta. It stated that among the repurposed drugs under consideration, this would be the suitable second option for rapid implementation in clinical trials.
The use of convalescent sera-serum obtained from someone who has recovered from an infectious disease and considered to be especially rich in antibodies against the infectious agent of the disease could also be an option, said the expert group. However, the report added: “...but it remains to be defined if sufficient amounts of sera with high antibodies titres could be feasibly collected, using concentration and purification processes.”
See also
Medical education and research: India
Institute of Post Graduate Medical Education and Research, Kolkata
Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER), Puducherry
