Medical malpractice: India
(→Guidelines) |
|||
| Line 9: | Line 9: | ||
|} | |} | ||
| − | + | ||
| − | + | ||
| − | + | ||
| − | + | ||
=Introduction= | =Introduction= | ||
| Line 114: | Line 114: | ||
| + | =Sex between doctor, patient= | ||
| + | ==Unethical even if consensual: MCI== | ||
| + | [https://epaper.timesgroup.com/Olive/ODN/TimesOfIndia/shared/ShowArticle.aspx?doc=TOIDEL/2019/04/18&entity=Ar00907&sk=2A1869D0&mode=text Chaitanya.Deshpande, April 18, 2020: ''The Times of India''] | ||
| − | [[Category:Crime|M MEDICAL MALPRACTICE: INDIA | + | |
| + | Sexual activity between doctor and patient, even if consensual, will be against good medical practice, says the ‘guidelines on sexual boundaries for doctors’ adopted by the Medical Council of India (MCI). Even if it is the patient who attempts to initiate it, it will be unethical for a doctor to enter into such a relationship. A relationship with a former patient too is discouraged and can be construed unethical. | ||
| + | |||
| + | |||
| + | The guidelines, framed by the Indian Psychiatric Society, are gender neutral and have been posted on the MCI website. | ||
| + | “We were forced to form some guidelines after the Delhi high court questioned us about MCI’s rules against sexual misconduct. It was acting after taking suo motu cognisance of a case involving a doctor of Indian origin in the US in 2017. The doctor was earlier registered with MCI. The court directed us to adopt the existing guidelines of IPS after examining them,” a member of MCI’s ethics committee told TOI. | ||
| + | However, academicians, said there was nothing new in the guidelines. Many of these points are taught in medical ethics and medical etiquette to every doctor during their MBBS course, said Dr Ajit Pathak, controller of examination, Maharashtra University of Health Sciences. | ||
| + | |||
| + | [[Category:Crime|M MEDICAL MALPRACTICE: INDIAMEDICAL MALPRACTICE: INDIA | ||
MEDICAL MALPRACTICE: INDIA]] | MEDICAL MALPRACTICE: INDIA]] | ||
| − | [[Category:Health|M MEDICAL MALPRACTICE: INDIA | + | [[Category:Health|M MEDICAL MALPRACTICE: INDIAMEDICAL MALPRACTICE: INDIA |
MEDICAL MALPRACTICE: INDIA]] | MEDICAL MALPRACTICE: INDIA]] | ||
| − | [[Category:India|M MEDICAL MALPRACTICE: INDIA | + | [[Category:India|M MEDICAL MALPRACTICE: INDIAMEDICAL MALPRACTICE: INDIA |
MEDICAL MALPRACTICE: INDIA]] | MEDICAL MALPRACTICE: INDIA]] | ||
| − | [[Category:Law|M MEDICAL MALPRACTICE: INDIA | + | [[Category:Law|M MEDICAL MALPRACTICE: INDIAMEDICAL MALPRACTICE: INDIA |
MEDICAL MALPRACTICE: INDIA]] | MEDICAL MALPRACTICE: INDIA]] | ||
Revision as of 21:21, 18 October 2020

This is a collection of articles archived for the excellence of their content. |
Contents |
Introduction
Raj Chengappa
November 15, 2013
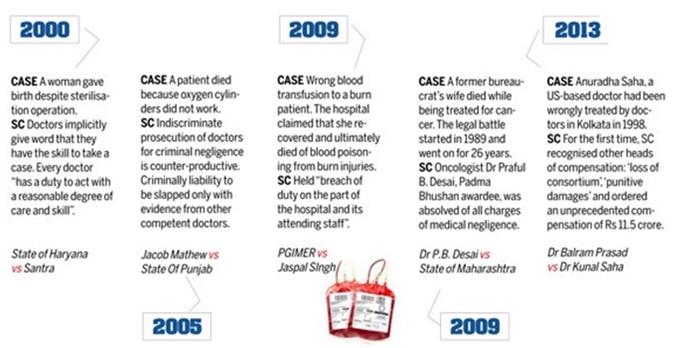
For years, the medical profession in India had neglected the warning symptoms. Shielded by flaccid regulatory authorities and a near comatose judicial system, the four lakh-strong community of doctors was almost immune to charges of malpractice.
Even when the problem grew to serious proportions, they failed to resort to corrective surgery. Now, aggrieved patients are beginning to wield the scalpel. Especially after a ruling made by the National Consumer Disputes Redressal Commission that medical services were liable under the powerful Consumer Protection Act of 1986.
Here's an alarming statistic: 98,000 deaths from medical injuries occur in India every year, reports an ongoing NABH study. Here's another: medico-legal cases have gone up by 400 per cent in the Supreme Court in the last 10 years, according to legal resource, Manupatra. Patients are afraid of an uncaring medical system. Doctors are terrified of assertive patients. Hospital life is under scrutiny, and with it the authority and autonomy of doctors. "Doctors are afraid," says Dr Arvind Kumar, chief of robotic and chest surgery at Sir Ganga Ram Hospital in Delhi. "The trust factor between doctors and patients is slowly coming down and there is no solution in sight."
"Negligent doctors need to be punished. But medical errors are also often 'system errors' and not the result of an individual physician's negligence," says Dr K. Srinath Reddy, former head of cardiology with AIIMS and currently president of Public Health Foundation of India. The scientific basis of good clinical practice depends on combining a well-gathered history of illness, physical signs and results of tests into an estimation of probabilities of possible diagnoses, he explains. While medicine is not an exact science, which always gives a 'yes' or 'no' answer, the 'art' of medicine lies in converting scientific evidence to standard management guidelines created by expert bodies, for all practitioners to follow. "Apart from minimising errors and avoiding unnecessary tests and treatments, adherence to guidelines forms the best defence against allegations of medical negligence," he adds.
The buzz among doctors is also on crippling compensations. In the latest issue of the British Medical Journal, Indian doctors have come head to head. "In India, healthcare is supposed to be regulated by a quasi-judicial medical council that has failed to protect against widespread negligent and irrational treatment," writes Dr Kunal Saha, a US-based doctor who received 'historic' justice-an unprecedented compensation of Rs.11.5 crore-in October 2013, for medical negligence that caused his 36-yearold wife Anuradha's death in 1998. "Large payouts awarded by the courts of law may be the only way to instill accountability for wayward doctors and to save lives."
A bench of Justices Dalveer Bhandari and H.S. Bedi had pointed out the need to protect doctors from "malicious prosecution": "It is our bounden duty and obligation of the civil society to ensure that medical professionals are not unnecessarily harassed or humiliated so that they can perform their professional duties without fear and apprehension."
Change will require looking at medical practice and malpractice in a new light: not just at material costs, but that the trust that exists between patients and doctors remains sacred.
Compensation for medical negligence
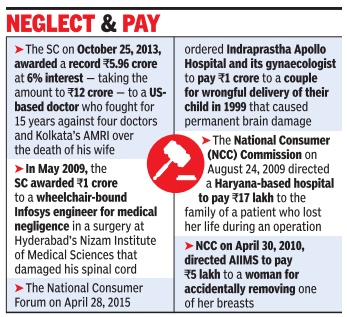
The Times of India, Jul 02 2015
SC awards Rs 1.8 crore to teen blinded as baby by doctors
Dad fought for 18 years after getting just Rs 5L
Dhananjay Mahapatra
Ordering a 36-fold 4 increase in compensation, the Supreme Court asked the Tamil Nadu gov ernment and a state-owned hospital at Egmore in Chennai to pay Rs 1.80 crore to the parents of a child who had lost her eyesight within a year of birth 18 years ago due to the negligence of doctors. The child was born 10 weeks prematurely to V Krishnakumar and his wife in August 1996 at the government hospital for women and children. But the neonatal expert and the paediatrician at the hospital never warned the parents that all babies born prematurely were prone to retinopathy of pre maturity (RoP) and that if early preventive measures were not taken, it could re sult in blindness. The parents visited US for surgery But the light in her eyes could not be restored, which had gone out because of medical negligence at the government hospital at the time of her birth. Krishnakumar filed a case under Consumer Protection Act in February 1998 before National Consumer Disputes Redressal Commission in New Delhi seeking Rs 20 lakh towards airfare, medical expenses and stay in the US, Rs 30 lakh towards future treatment and Rs 50 lakh for pain, loss and mental agony .
Though a medical team from AIIMS confirmed negligence on part of the hospital and the two doctors, the national commission awarded just Rs 5 lakh as compensation.
Appearing for Krishnakumar, advocate Nikhil Nayyar argued that the commission failed to take into account the actual expenses incurred by the parents for the treatment of the girl. Nayyar also said the award failed to consider the money required for future treatment and compensation for the prolonged period of mental agony of the child and her parents.
A bench of Justices J S Khehar and S A Bobde ordered the state and other respondents to pay Rs 1.38 crore as compensation and Rs 42 lakh as reimbursement of medical expenses, taking the total award to Rs 1.80 crore.
Guidelines
Patients' consent essential before invasive procedures
Holding that a patient has an inviolable right with regard to his or her body , the National Consumer Disputes Redressal Commission has said that doctors must take consent of a patient or his family members for any invasive procedure during treatment.
A bench of Justice Ajit Bharihoke and Anup K Thakur said provision of taking consent could be overlooked only if urgent intervention was required to save the life of a patient. It held Delhi-based Hospital Sitaram Bhartia Institute of Science and Research guilty of negligence by not taking consent before inserting a catheter for central venous line procedure on a patient and directed it to pay a compensation of Rs 7 lakh to him.
“Unless the procedure is necessary in order to save the life or preserve the health of the patient and it would be unreasonable to delay the procedure until the patient regains consciousness and takes a decision, a doctor cannot perform such procedure without consent of the patient. In the instant case, the insertion of catheter by Central Venous Line procedure being an invasive procedure carrying certain risk of complication, including injury to the jugular vein or bursting of the blood cells, the team of doctors was legally required to obtain consent of the patient,“ it said.
Advocate Nikhil Jain, appearing for the patient, contended that the doctors had not taken consent of family members and alleged that due to their negligence, the jugular artery was ruptured resulting in profuse bleeding and he had to be shifted shift to another hospital for treatment.
The hospital, however, said procedure of insertion of CVL in the patient's neck was a routine procedure like giving injection and consent was not required as it was not a surgical or invasive procedure.
Refusing to accept its plea, NCDRC said there was no merit in the contention and putting CVL in the body of a patient could not be equated with ordinary procedure.
“A central venous catheter (CVC) al so known as central venous line or central venous access catheter, is a procedure in which catheter is placed into a large vein. A catheter can be placed in veins in the neck, chest, groin or through veins in the arm. It is used to administer medication or fluids that are unable to be taken by the mouth. From the record it transpires that in the instant case, the CVC was tried to be placed by the team of doctors in the internal jugular vein, which went wrong resulting in injury to the vein and excessive bleeding. The aforesaid procedure obviously is an invasive procedure which admittedly carries the risk,“ it said.
“It is not the case of the hospital that there was an emergency threatening the life of the complainant, which could justify the procedure to save the life without seeking consent,“ it said.
The hospital, however, said it may approach the Supreme Court. “We haven't received the copy of the order yet.After seeing the order, if order is adverse we will approach the Supreme Court,“ said Dr Shubhra Verma, General Manager (Operations), Sitaram Bhartia hospital.
Removal of uterus to save life not medical negligence
In a landmark judgment, the National Consumer Disputes Redressal Commission (NCDRC) – the apex body of consumer disputes redressal in the country – has held that if hysterectomy is done to save the life of a patient, then it is not medical negligence and denied compensation to a woman who said removal of uterus had deprived her of becoming a mother again.
In 2002, a woman’ uterus was removed post childbirth owing to her medical complications. She moved NCDRC seeking Rs 35 lakh compensation from the doctors who performed the surgery on the ground that she had been deprived of becoming a mother in future.
A bench of Dr S M Kanitkar and Dinesh Singh noted both the mother and child then born were leading a normal life. “We do not find any deficiency/negligence in removal of uterus, as it was essential in that condition to save the life of the patient – mother,” the bench said.
The commission further stated that as the patient’s ovaries had been left intact, she hadn’t lost the her chance to have another child totally as it was possible through advanced medical techniques like assisted reproductive technology or surrogacy.
In her complaint, the woman alleged that the consent of her family members was not obtained by the doctors before the removal of her uterus. It was also claimed that her attendants were humiliated by the doctors and their staff.
The doctors, on the other hand, denied any deficiency or negligence on their part. As per their claims, they had conducted a normal delivery and a healthy child was born. During the procedure of suturing, the woman’s condition deteriorated. Despite their efforts to stop uterine bleeding, the doctors were unable to control it. By then the woman’s condition had turned serious. Her life had to be saved at any cost, the doctors said. “Therefore, the emergency hysterectomy was performed. It was not a medical negligence,” it was submitted. The commission found the complaint to be “frivolous and vexatious”. It said, “We are, however, refraining from imposing cost.”
Leaving piece of drill in patient tolerable
A consumer forum has absolved a doctor of the charge of medical negligence for inadvertently leaving a fragment from a drill, which broke off during surgery , in a patient's elbow. The forum quoted medical texts to say that instruments break during operations, and that the fragments left behind are “well-tolerated by the human body“, adding that additional surgery to remove them is not justified. Petitioner V Vasudevan had moved the district consumer disputes redressal forum against Dr Sudhakar Williams, seeking
compensation for medical negligence.
Vasudevan said he was admitted to Dr Rangarajan Memorial Hospital, Anna Nagar West, after an accident in April 2009. Around 30 months after the surgery on his right elbow, Vasudevan, who said he suffered continuous pain in its wake, consulted another doctor. An X-ray of the elbow showed a fragment from the drill lodged in his bone, and Vasudevan underwent surgery in another hospital to have it removed. In his defence, Williams said Vasudevan experienced pain because of injuries sustained in the accident. The doctor's counsel said that medical literature stated it was common for small pieces of the surgical drill to break and get lodged in the bone.
A bench comprising forum president K Jayabalan and member T Kalaiyarasi noted that Vasudevan had not provided any evidence to prove that the fragment caused him any injury .
Sex between doctor, patient
Unethical even if consensual: MCI
Chaitanya.Deshpande, April 18, 2020: The Times of India
Sexual activity between doctor and patient, even if consensual, will be against good medical practice, says the ‘guidelines on sexual boundaries for doctors’ adopted by the Medical Council of India (MCI). Even if it is the patient who attempts to initiate it, it will be unethical for a doctor to enter into such a relationship. A relationship with a former patient too is discouraged and can be construed unethical.
The guidelines, framed by the Indian Psychiatric Society, are gender neutral and have been posted on the MCI website.
“We were forced to form some guidelines after the Delhi high court questioned us about MCI’s rules against sexual misconduct. It was acting after taking suo motu cognisance of a case involving a doctor of Indian origin in the US in 2017. The doctor was earlier registered with MCI. The court directed us to adopt the existing guidelines of IPS after examining them,” a member of MCI’s ethics committee told TOI.
However, academicians, said there was nothing new in the guidelines. Many of these points are taught in medical ethics and medical etiquette to every doctor during their MBBS course, said Dr Ajit Pathak, controller of examination, Maharashtra University of Health Sciences.