National Capital Region (India): Health
This article has been sourced from an authoritative, official readers who wish to update or add further details can do so on a ‘Part II’ of this article. |
Contents |
The source of this article
Draft Revised Regional Plan 2021: National Capital Region
July, 2013
National Capital Region Planning Board, Ministry of Urban Development, Govt. of India, Core-4B, First Floor, India Habitat Centre, Lodhi Road, New Delhi-110003
National Capital Region Planning Board
National Capital Region (India) : HEALTH
Background
Health Infrastructure is an important indicator to understand the healthcare delivery provisions and mechanisms in the region. Health facilities in India is structured at three levels namely primary (Sub Centre and Primary Health Centre), secondary (District Hospital and Community Health Centre) and tertiary (Nursing homes, speciality and super-speciality hospitals) based on population norms. Health infrastructure in the urban areas is different from the rural areas. In urban areas mostly two types of health infrastructure are provided i.e. Hospitals and Dispensaries, while rural areas have the Community Health Centers at the Secondary level and Primary Health Centers, Sub Centers and Village Health Guides & trained Dais at Primary level.
EXISTING HEALTH FACILITIES IN NCR
12.5.1 Health facilities:
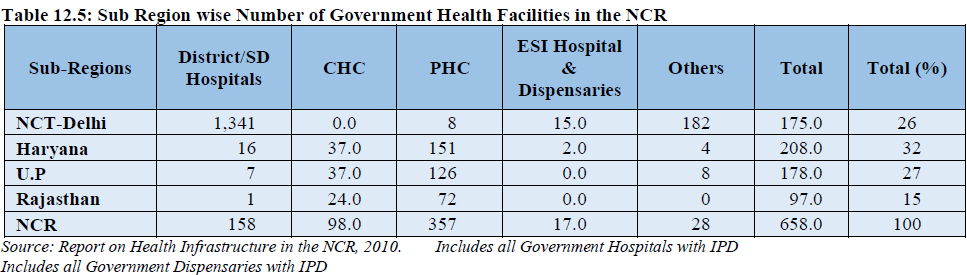
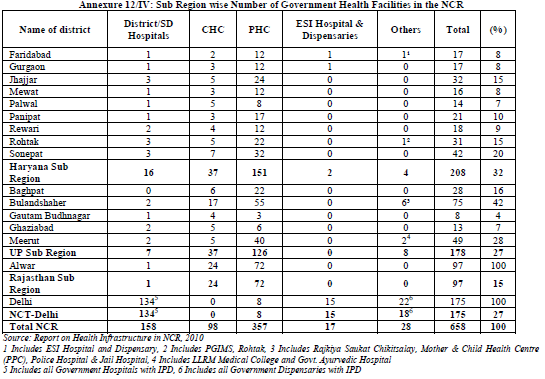
A total number of 658 Government Health facilities are available in the NCR including NCT-Delhi. Haryana sub-region has the highest number of health facilities accounting for 32 percent followed by UP Sub-region and NCT-Delhi having 27 percent each. Rajasthan sub-region has the lowest share of 15 percent (Table 12.5).
As per report on Health Infrastructure in NCR (2010) regarding level of facilities, Haryana sub-region has the largest number of primary level facilities (151) accounting for 42% of total PHC in the region closely followed by UP Sub-Region having 35%, Rajasthan sub-region has 20% while NCT-Delhi has 2%. On the other hand in terms of tertiary level medical care i.e. district hospital and multi specialty hospitals. Delhi has a maximum number of 134 accounting for 85% whereas Haryana Sub-Region has only 10% and UP Sub-Region 4%.
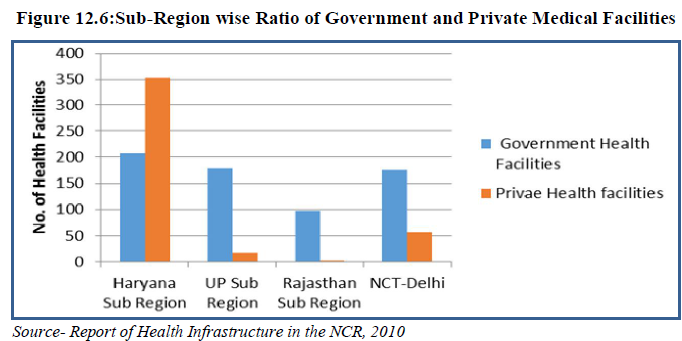
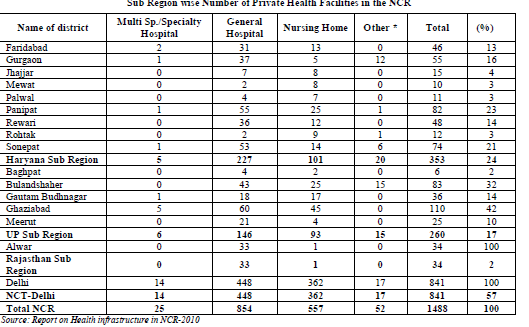
More than half of the private health facilities accounting for 56.5% are concentrated in the NCT-Delhi (Table 12.6 & Fig 12.5). Haryana sub-region and UP sub-region have 23.7% and 17.4% concentration of private hospital while Rajasthan sub-region has two lowest number of private hospital with a share of only 2 %. The ratio of government to private health facilities in the NCR is 1:2.2.
Apart from NCT Delhi, multi and super-speciality private hospitals are available in Faridabad, Gurgaon, Panipat & Sonepat districts of Haryana sub-region and GB Nagar & Ghaziabad districts of UP sub-region (Annexure 12/IV).
Districts like Jhajjar, Mewat, Palwal, Rohtak and Baghpat have limited number of private health facilities as compared to others. NCT-Delhi has the highest ratio of 1: 4.8 followed by Haryana sub-region and UP sub-region with a ratio of 1:1.7 and 1:1.4 respectively. In Rajasthan sub-region private hospitals are less than government hospitals and the ratio is 1: 0.4 (Fig 12.6).
12.5.2 Number of beds available in the NCR:
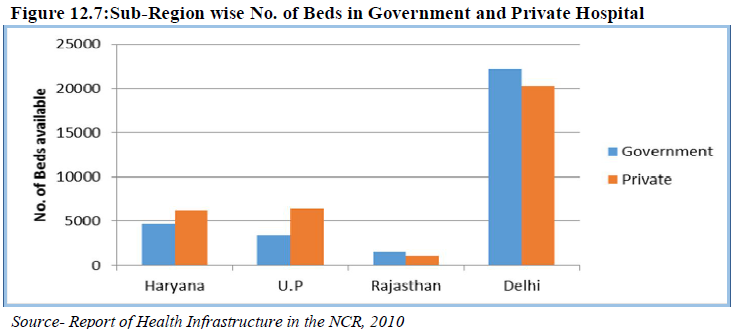
The total number of inpatient beds in the NCR is 65,803, out of which 48% beds are available in the government health facilities with an average occupancy rate of 61 percent. A total number of 34,126 (52%) in-patient beds are available in private facilities of NCR sub-regions with an average occupancy rate of 46 percent. This shows that although the numbers of beds are more in the private sector the rate of occupancy is low mainly because of affordability (Table 12.7).
At sub-regional level except in Rajasthan sub-region and NCT-Delhi proportion of beds are more in
private hospitals than government hospitals. In government hospitals occupancy rate in NCT-Delhi is the
highest (72%) followed by Rajasthan sub-region with 69 % and UP sub-region with 57 % while in
Haryana sub-region it is 47%. Utilization level of beds in private hospitals is also the highest in Rajasthan
sub-region with 62 % whereas in other sub-region it is below 50% (Fig 12.7).
Ambulance facility
The average number of ambulance available per health facility (like Hospitals, Health Care Centers, and Nursing Homes etc) is highest (2.1 per health facility) in the government sector in NCT Delhi. Availability of ambulances is poor in the Government sector hospitals, in case of UP Sub Region (0.3 per health facility) and Rajasthan Sub Region (0.2 per health facility). On the other hand, one general care ambulance is available per private hospital in Uttar Pradesh Sub Region. The number of trauma ambulances is insignificant in government sector of NCR other than NCT Delhi.
Use of Medical Facilities
Bed utilization is sub-optimal in most of the health facilities, while some hospitals are becoming overcrowded. Except in NCT Delhi the private health care centers are more equipped with medical facilities than the government ones in the NCR. In all it can be highlighted that 7% of the Government and 17% of the private health care centers have blood storage facilities and 19% of the government and 21% of private facilities have Histopathology test facilities.
AYUSH
Among different categories of AYUSH medical facilities Ayurveda is the most common. A total number of 226 Ayurveda specialists are providing consultations to the patients in various NCR sub-regions. Out of them, 200 are available in Government facilities. Majority of them are available in health facilities of Delhi and Uttar Pradesh. The Government facilities in Alwar District of Rajasthan have about 40 Ayurveda specialists. The next popular AYUSH category is Homeopathy. There are a total of 123 homeopaths in NCR out of which 68% are in Delhi. Also in Delhi private and government health facilities have equal number of homeopaths. There are 11 Yoga, 1 Siddha and 85 Unani specialists in NCR, of which majority are available in Delhi.
Referral Hospitals
As part of the study on Health Infrastructure in NCR, an analysis of 11 referral Hospitals of NCR was carried out to assess the existing infrastructure available in these facilities and to study the profile of the patients receiving treatment. Eleven Referral Hospitals selected for the study comprises 45% government Social Infrastructure 179 and 55% private facilities. Category wise, 2 facilities are General-Tertiary care hospitals, while rests nine are Speciality or Super Speciality Hospitals. The major findings from the study are:
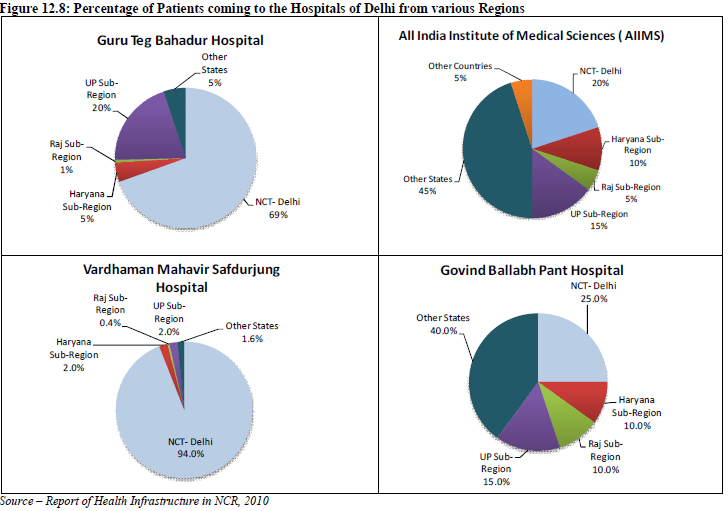
A. Inflow of Patients to the Referral Hospitals of the NCR The super speciality hospitals of Delhi like AIIMS, GB Pant Hospital etc have larger share of patients coming from other states outside NCR region (Approx. 40%), whereas Safdarjung hospital and tertiary care government hospitals (like Guru Teg Bahadur Hospital) receives 5-10 percent outside NCR patients and the largest share (60-70%) of patients to these hospitals are from Delhi (Figure 12.8).
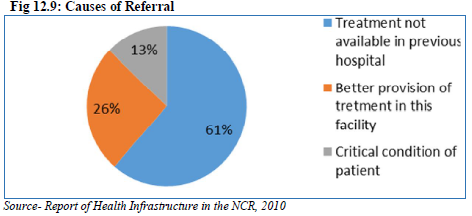
Similarly, the hospitals of the Haryana Sub region receives a majority of the patients from within the state itself and approximately 10-15% comes from the other sub regions of the NCR (Delhi, UP, Haryana, Rajasthan). Haryana Sub Region contributes 30 percent patients, half of this come from Gurgaon district. The hospitals of the UP Sub Region receive half of the patients from UP Sub Region, while 15 percent come from Delhi another 5-15 percent come from other states – generally Bihar, Uttarakhand and J&K. Rest 20-25 percent patients come from NCR districts of Haryana and Rajasthan Sub Region. The study has highlighted that about 32 percent of 584 patients interviewed were referred from other health facilities and the rest 68 percent came directly to the facility. B. Causes of Referral About 61 percent of referred patients have informed that the required treatment was not available in the previous hospital, while 13 percent were critical cases. Better provision of treatment in the referral hospitals is the reason of referral for 26 percent patients (Table 12.8 and Fig. 12.9).
C. Ailments for which referred The major ailments for which patients come to Delhi from the UP Sub Region are – Cancer, Gynecological problems and Obstetrics, Pediatric problems, Neurological problems, and various types of fevers like malaria, typhoid etc. pulmonary problems, Gastro intestinal problems and ENT problems. It has been observed that 40 percent of the respondents randomly selected in referral Hospitals are not residents of Delhi. About a half of these outsiders are coming from NCT-Delhi while 7 percent are from districts of Haryana Sub Region and nearly 17 percent from non NCR districts of UP and rest from other states like, Bihar, Uttarakhand, West Bengal etc.
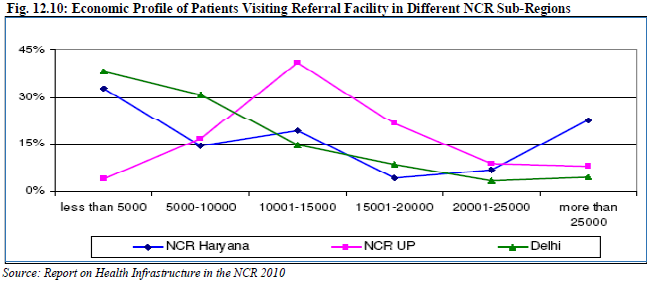
D. Economic profile of Patients The study shows that proper treatment for people belonging to lower income group is not adequate in NCR sub regions outside Delhi and considerable percentage of them come to NCT- Delhi to avail the facilities offered by the government referral hospitals (Fig. 12.10). 12.7 Need Assessment and Gap Analysis: For the purpose of assessment of required health facilities and the existing gaps, the estimated population and decadal growth rate of each district and sub regions were calculated, up to year 2021 in an interval of five years from 2011. These estimations were made on the basis of the population as per Census 2001 and 2011.
Looking into the sub region wise distribution of available population, it is evident that NCT Delhi is having about 36.4 percent of the total population followed by Uttar Pradesh (32%), Haryana (24 %) and Rajasthan (8%)
Need assessment of Hospital beds in the NCR
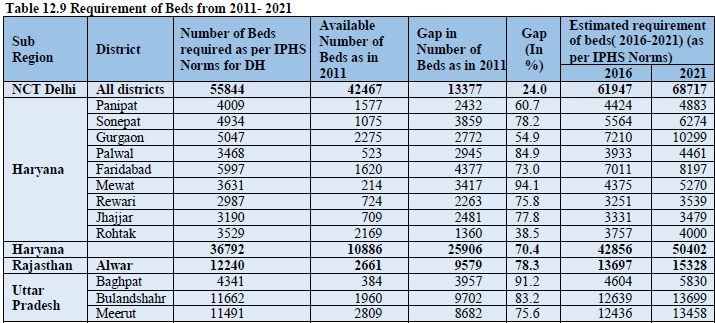
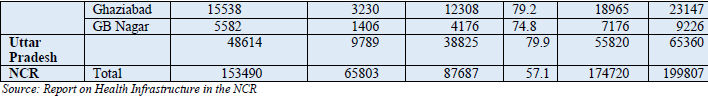
After analysing different norms, it is observed that as per WHO, 5 beds are required for 1000 persons and as per Indian Public Health Standards (IPHS), the requirement is 3.33 beds per 1000 persons. IPHS norm is found more suitable for hospitals in NCR as most part of the region is urban.
Tables 12.9 provide details of requirements of beds in different sub regions of NCR considering bed population ratio as per IPHS norms for District hospital that is 3.33 beds per 1000 persons. Looking into sub region wise need it could be concluded that the gaps in availability of beds is more in the Uttar Pradesh Sub Region which is currently having 20 percent of its required beds strength followed by Rajasthan having 22 percent of required beds and Haryana about 30 %. (Fig. 12.11).
To meet the bed requirements NCR needs about 2.3 fold increase in its beds strength by 2021. Looking into sub region wise distribution of required beds the Uttar Pradesh Sub Region needs about 5 fold increase in present situation which will need a leap of 6.5 folds if considered for 2021.
Policies and Proposals
i. The analysis of the data reveals that the private sector health care provision in urban areas is greater than that of the public sector and also the medical facilities in the private facilities are more than the public sector. It is suggested that IPHS norms should be followed so that the burden on tertiary care can be minimized. Provision for location of health facilities needs to be followed as per norms of National Urban Health Mission. ii. To cater to the medical needs of the rural areas mobile medical vans could be introduced. These mobile vans equipped with basic medical facilities could supplement a primary health centre and travel to those areas where the primary health centers do not exist or have failed to meet the requirements of the people. These vans could have a schedule of visits in particular areas and could also be called in times of emergency.
iii. It is observed that the three tier-systems of Health services is not functioning effectively thereby leading to overburdening of higher level of health care facility i.e. Tertiary care. The institutional framework of the entire health system should be strengthened by introducing systematic monitoring as required under National Urban Health Mission. iv. In a situation where there is a paucity of qualified healthcare personnel, the most optimal solution is distance healthcare (also including telemedicine, tele-consulting and telecounselling) where expert advice can be made available at some central point and accessed as and when required by telephone or internet. v. Tele-Preventive Medicine can also be used, the term ‘tele-preventive medicine’ is defined as the use of the internet to collect information from large number of people (both healthy and sick) to prevent outbreak of disease.
1997-2017: alcohol use, obesity, BP rise
DurgeshNandan Jha, Delhi `enjoying' life, but losing its heart, April 18, 2017: The Times of India
See graphic.

Epidemic Of Cardiac Diseases Likely: Docs
A unique set of data generated by Indian researchers has put numbers to a trend physicians have been warning about for long -Delhi-NCR is heading towards an epidemic of cardiovascular diseases (CVD), chiefly heart attack and stroke cases, due to increase in prevalence of alcohol use, obesity and raised blood pressure (BP) over the past 20 years. And the trend has been vis ible among both urban middle class and their rural counterparts, said doctors. Alcohol use, for example, has gone up from 16.1% to 25.6% among urban dwellers. In rural areas, the increase is nearly four times -from 8% to 33.2%.
Prevalence of body mass index (BMI) and BP , two other risk factors for cardiovascular diseases, among urban men and women aged 35-64 years, has gone up from 24.4kgm2 to 26kgm2 and 121.274.3mmhg to 129.883.9mmhg, show the data published in the latest issue of Global Heart, a reputed medical journal.
The surveys were conducted in two phases to find the 20year trend for cardiovascular disease (CVD) risk factors.“For the urban data, we went to households in whole of Delhi. Rural data was collected from Ballabgarh blocks of the adjoining state of Haryana,“ said D Prabhakaran, an epidemiologist who led the research. Endocrinologists, car diologists and community medicine specialists from AIIMS were also part of the research group.
A person with BMI over 25kgm2 is defined as overweight and at risk for CVD.Similarly, those having BP levels above 14090mmhg are considered at risk for CVD which is defined as group of disorders of the heart or blood vessels, and include mainly hypertensive, ischaemic, rheumatic and cerebrovascular heart disease or strokes. It is estimated that one in every four deaths in India is attributable to CVD. If steps are not taken to prevent the risk factors from increasing, morbidity and mortality due to CVD may go up, said Prabhakaran.
India has witnessed a rapid economic transition since 1991. Researchers said that post-liberalisation, the country saw rapid urbanisation, rural-to-urban migration, and changes in diet and lifestyle that could be behind the increase in prevalence of risk factors for CVD.
“We need an inter-ministerial approach to fight this impending crisis of CVD epidemic.While the health ministry can work on infrastructure growth for timely screening and treatment of patients with CVD, the urban development ministry can come with planning for more space to play and walk so there is increased physical activity and the HRD ministry can come up with awareness campaign in schools to publicise preventive steps at school and college level,“ said Dr Nikhil Tandon, head of the endocrinology department at AIIMS who was also part of the study. The age at which CVD strikes has also come down, he said.