Cancer: India
This is a collection of articles archived for the excellence of their content. |
Breast cancer
Chemical in toiletry items causing breast cancer
[ From the archives of the Times of India]
Found in make-up, toothpastes & also food products
Scientists say they have discovered a chemical, used in daily toiletry products and food products, in tumours of 40 breast cancer patients, but allayed fears by claiming that further probe is needed.
A team at the University of Reading claims the chemical compound, called parabens, was spotted in the tissue samples of the 40 women undergoing mastectomies between 2005 and 2008 for first primary breast cancer in the UK. Parabens possess oestrogenic properties. Oestrogen is known to play a central role in the development, growth and progression of breast cancer.
Parabens are found in moisturisers, make-up, shaving foam, tanning lotions and toothpaste, as also used in processed meats such as sausages, pies and pastries along with other savoury snacks. For the study, altogether 160 samples were collected, four from each woman. The scientists found 99% of the tissue samples contained at least one paraben and 60 per cent of the samples had five, the ‘Daily Mail’ reported.
The team found women who didn’t use underarm deodorants still had measurable parabens in their tissue, suggesting they must enter the breast from other sources. Dr Philippa Darbre, who led the team, said: “The fact that parabens were detected in the majority of the breast tissue samples cannot be taken to imply that they actually caused breast cancer in the 40 women studied. However, the fact that parabens were present in so many of the breast tissue samples does justify further investigation.” Added co-author Lester Barr from the University Hospital of South Manchester: “Our study appears to confirm the view that there is no simple cause and effect relationship between parabens in underarm products and breast cancer.” PTI
Birla Hospital: Blind women detect breast cancer
Ambika Pandit, August 15, 2019: The Times of India
Blind women use touch to detect breast cancer
NEW DELHI: Using their power of touch, five blind women over the last four months have been able to detect pre-cancerous or cancerous lesions in around 17 women (or 3.5% of over 500 women examined) in C K Birla Hospital for Women in Gurgaon. Their findings were affirmed medically by radiological tests — mammograms and ultrasounds.
These outcomes draw attention towards the need for early detection of cancer through regular examinations. This first of its kind study claims high levels of sensitivity through physical examinations carried out by visually impaired women especially trained using tactile strips to map every centimetre of the breast. The Medical Tactile Examiners (MTEs) are able to detect lumps as small as 0.5 milimetres.
Voluntary organisation National Association for the Blind’s Centre for Blind Women in Delhi started training women to be MTEs last year to empower them professionally and financially. The nine-month course is being conducted in collaboration with German gynaecologist Dr Frank Hoffmann’s project “Discovering Hands”.
The training has been certified by Rehabilitation Council of Germany. Of the first group of seven MTEs, two were taken up by Fortis Hospital in Vasant Kunj and five by C K Birla Hospital for women in Gurgaon. Another batch of seven will soon be ready as MTEs.
As per data from C K Birla Hospital, nearly 900 women from Delhi and NCR underwent ‘Tactile Breast Examination (TBE)’ along with ultrasound breast for those below 40 years and mammogram for those above 40 years of age. In the last four months over 500 women were studied to evaluate the enhanced touch (Tactile Sensation) of a visually impaired MTEs.
The clinical findings of the study shared by Dr Mandeep S Malhotra, director, The Breast Centre at C K Birla Hospital for Women show that the MTEs have a very high level of sensitivity for detecting breast lesions. “Of the 500 cases examined, the MTEs reported 70% as normal and detected changes in breasts of 30% women. Radiological examinations affirmed the findings with 70% women found to be normal. Of the 30% with changes in breasts it turned out that in 15% there were non-specific changes like fibro cysts, 11.5% had benign breast lesions and around 17 women (3.5 %) had lesions that were either cancers or pre-cancers,” Dr Malhotra said.
“Less than 2%, women, were into any kind of active breast screening and during follow-up said they had started doing self breast examination and would continue with regular check-ups,” Dr Malhotra added. He, however, cautioned that MTEs were not a substitute for radiological testing but a supplementary check that mapped the entire breast area through a physical examination.
Dr Malhotra cited national statistics to point out that early detection was the need of the hour. “Breast cancer is the most common cancer among women in India. Every year around 1.5 to 2 lakh new women are being diagnosed with breast cancer. As per ICMR data in urban areas 1 in 22 women are likely to be affected by breast cancer. 50% of them don’t survive beyond five years of the diagnosis,” he shared.
According to American Cancer Society Guidelines, the standard screening process of mammography, should start at the age of 45. “Breast cancer in Indian women is a decade younger in comparison to western women with peak incidence at 40– 50 years and Indian women have inherently higher breast density. Both the facts suggest limited application of screening mammography in Indian settings,” Dr Malhotra shared.
In this study of 500 cases, more than 70% feared breast cancer, but were unaware of what should be done. In 30 to 40% cases the woman above the age of 40 who underwent mammogram needed an ultrasound correlation, suggesting limited applicability of mammogram. “The good thing is that a check-up by an MTE can be done for women of all age groups. The focus should be on steering younger women towards prevention,” Dr Malhotra added.
Cancer amongst children
2016, Childhood cancer campaign
The Times of India, Sep 23, 2016
Aditya Dev
Cancer awareness programme held at Taj on September 25-27
In a unique initiative, "CanKids..Kidscan", a national society for change for childhood cancer in India, has joined hands with the Archaeological Survey of India (ASI) and UP government to hold an exhibition at the Taj Mahal from September 25 to 27. The exhibition is a part of the NGO's 'Go Gold India - Taj Goes Gold and UP Goes Gold campaign', aimed at spreading awareness about childhood cancer.
Earlier the organizers had requested the ASI to lit up the Taj "gold" for this event on the lines of several monuments and installations in many parts of the world turned gold in September 2015 to express their solidarity with childhood cancer awareness, but there being a Supreme Court order against holding any such activity within the Taj's premises, ASI collaborated with them to hold an exhibition at the monument instead.
ASI superintending archaeologist Bhuvan Vikrama said, "The exhibition will be held near the Royal gate of the monument. Our team will also be there and spread awareness about the cause." A spokesperson of the NGO told TOI that it would be the first time that such a cause related exhibition held at the Taj Mahal.
During the three-day exhibition, Taj Mahal replicas decorated by children with cancer at 35 participating cancer centers. In addition to that 'I Deserve' competition posters, where children have expressed their demands, and wished for better treatment and care, right to education, clean environment, play school in the hospital ward, no restriction on their movement and most importantly their childhood will be displayed. As many as 10 best pledge books (in which 2,50,000 signatures from across India, to make childhood cancer a health priority) will also be on display.
The spokesperson of the NGO said, "The aim of the exhibition will be to raise awareness about childhood cancer and gold as the colour of childhood cancer. We will also raise funds for children with cancer, survivors and their families and seek Central and state governments support for childhood cancer to be distinct part of cancer control plans, policy and programs and a child health priority in India."
2017 Incidence much lower than in West
July 30, 2019: The Times of India
‘Rate of cancer in India’s kids much lower than that in West’
A Lancet study has pointed out that 82% cancer cases among children come from poorer countries. However, there are two bright spots as far as India is concerned. “First, there are centres such as Tata Memorial Hospital in Mumbai, AIIMS in Delhi or PGI in Chandigarh where survival rates are almost equal to the western figure,” said Banavali. Second, the incidence or rate of cancer among India’s children is much lower than in the West. “The incidence of cancer among children in India is 80-90 children per 1,00,000 children; the corresponding figure for the US and Europe is 160,” added Banavali.
However, due to India’s huge population, even a smaller proportion translates into huge numbers in absolute terms. Moreover, unlike in the western countries, where the proportion of adult and paediatric population is almost equal, youngsters below 35 years account for over 65% of India’s population.
For the first time, the new Lancet study also quantifies the burden of paediatric cancer in terms of the number of health years lost for a country. “The number of new cancer cases in children and adolescents (0-19 years) is relatively low around 4,16,500 globally in 2017, but treatment-related ill-health and disability and fatal cancer are estimated to cause 11.5 million years of healthy life lost globally every year,” it said.
The GBD-Lancet study was conducted by St Jude Children’s Research Hospital, Memphis, and University of Washington in Seattle, and funded by Bill & Melinda Gates and others. “Lack of diagnosis, access to healthcare and a younger population are responsible for disproportionately large childhood cancer burden in many of the poorest countries,” the study said.
Causes
1990-2016, major causes

From: September 13, 2018: The Times of India
See graphic:
The top causes and types of cancer, 1990-2016
Cervical cancer
Tata Memorial Hospital’s cervical cancer trial

From: Sumitra DebRoy, 1.3L new patients a yr in India, only 580 radiotherapy centres, March 8, 2018: The Times of India
‘Docs Mustn’t Waste Time To Excise Tumour’
Tata Memorial Hospital’s cervical cancer trial involving 633 women has found that the fiveyear disease-free survival rate of second-stage patients who received a combination of chemo and radiotherapy was 77% as compared to 70% in those who were given chemotherapy followed by surgery. The trial clearly establishes non-surgical treatment as the better strategy for such patients.
The study has been published in the February edition of the Journal of Clinical Oncology. Removing surgery from the line of treatment would also make it more cost-effective, the researchers said. Apart from saving valuable time lost in deciding on treatment modalities, they said the findings should save scores of women from undergoing botched-up, unnecessary surgeries, including incomplete hysterectomies.
“There has always been an unsubstantiated belief that a tumour must be resected in order to treat cancer. But our study shows that in cases where the tumour was surgically removed, it did little to stop the disease’s progression or even contain it locally,” said Dr Supriya Chopra, professor of radiation oncology, TMH.
Every year in India, nearly 1.3 lakh women are detected with cervical cancer, while 70,000 succumb to it. At TMH, 100 cervical cancer patients come each year on average with a history of inappropriate treatment. Often doctors operate the tumour with little success, but in the process compromise a patient’s chances of responding optimally to radiotherapy.
Medical oncologist Dr Sudeep Gupta said the study has put to rest one of the longest standing controversies about the best way to tackle locally advanced cervical cancer. “If a tumour is more than 4cm, surgery is not the best option. There is a tendency among doctors to first shrink the tumour with chemotherapy and then go for surgery. Our study has proved that it’s not ideal and the standard way should be a combination of radiotherapy and chemotherapy.”
The findings put renewed focus on the lack of adequate radiotherapy facilities in the country. “Presently, merely 15-20% of patients get treated with radiation, whereas 60-70% of them need it,” said Dr Chopra. There are 359 external and 232 brachytherapy (internal radiation) facilities in India at present. “Most are in metro cities. Women, particularly those in villages, have little access to such facilities,” she said. “The trial’s findings will now be used to draw up a report on the infrastructure requirements for radiotherapy in India and presented to the government.”
A sister study led by Dr Shyam Srivastava and Dr Umesh Mahantshetty, radiation oncologists, TMC, published in JAMA Oncology, found that even in advanced cervical cancer-–stage 3—radiotherapy with simultaneous chemo is superior than radiotherapy alone. Gynaec-oncology surgeon Dr Amita Maheshwari said doctors routinely use surgical route on the grounds that radiation facilities are scarce, but this can no longer be accepted.
2016: Cervical cancer cases on decline
Sushmi Dey, July 22, 2019: The Times of India
Cervical cancer, the second most common cancer among Indian women, is on a declining trend with population-based registries across the country showing new cases falling at an average rate of 1.81%-3.48%, government data showed.
All the regional registries by ICMR (released in 2016) including Bengaluru, Barshi, Chennai, Bhopal, Delhi and Mumbai showed a significant decrease in age-adjusted rate over time.
While the reduction was attributed primarily to improvement in living standards of women, experts cautioned that the incidence rate could have been underestimated due to under-diagnosis, primarily in rural areas.
“In India, most cervical cancer cases are detected with regional spread of the disease, and a very small proportion is diagnosed at a localised stage. Hence, many cases may not be reported as cervical cancer at all,” a public health expert said.
The population-based cancer registry by ICMR estimated (for 2012-2014) the annual percentage change (APC) over time in incidence of cervical cancer in Bengaluru at -2.26%, Bhopal (-1.81%), Chennai (-3.48%), Delhi (-2.73%) and Mumbai (-1.99%). All these regions showed a significant decrease for annual average rate for three and five years.
Cervix is the second most common site for cancer in Indian women, preceded only by breast. More Indian women die of cervical cancer than in any other country in the world, and one quarter of the world’s cervical cancer burden is in India. Official estimates for 2012 showed that every year, 1,22,844 women were diagnosed with cervical cancer and 67,477 died from the disease.
The WHO estimated 5,30,000 new cases of cervical cancer globally (estimates for 2012), with approximately 2,70,000 deaths, representing 7.5% of all female cancer deaths. More than 85% of these deaths occurred in lowand middle-income countries. A study published in ‘The Lancet Oncology’ earlier this year said India could eliminate cervical cancer by 2079 by taking into account introduction of the human papilloma virus (HPV) vaccine and cervical cancer screening.
India plans to introduce HPV vaccine in the government programme by 2020, and has started screening for cervical cancer in health and wellness centres under the Ayushman Bharat programme.
Cost to nation
Cost to nation of avoidable cancer deaths in 2012: $6.7bn
Avoidable cancer deaths cost India $6.7bn in 2012, January 29, 2018: The Times of India
India may have low cancer rates as compared to western nations but it accounts for among the highest premature and avoidable deaths due to the disease. A study published last week states India and Brics colleagues Brazil, Russia, China and South Africa lose tens of billions of dollars in lost productivity due to cancer deaths.
Everyone’s work contributes to the economy, and not working represents a loss to society. Starting here, a study was undertaken as part of the European Short- Term Scientific Mission to assess the loss of productivity in Brics countries on account of cancer. It found that India recorded a total productivity loss of $6.7 billion in 2012 due to cancer, representing 0.36% of the GDP that year. This was second only to South Africa’s, which recorded a loss of $1.9 billion, amounting to almost 0.5% of its GDP.
The productivity lost per death in India was under $20,000 — the lowest among Brics countries. The greatest total productivity losses in — $0.74 billion — could be attributed to tobacco-related lip and oral cancers. Cancer claims seven lakh lives every year across India, with another 10 lakh new cases detected annually. “The use of smokeless tobacco, often combined with betel quid, can be attributed to almost 50% of oral cavity cancers in India. Lip and oral cancers dominate lost productivity in India due to the relatively high prevalence of chewing tobacco. We know that tobacco results in healthcare costs of up to Rs 100,000 crore annually,” said Dr Pankaj Chaturvedi, professor of head and neck cancer at Tata Memorial Hospital in Mumbai.
The loss of productivity in Brics economies due to cancer-related premature mortality is considerable in total cost terms — $46.3 billion, which represents 0.33% of their combined GDP. Many of the cancers that result in deaths in the Brics countries are “amenable to prevention, early detection or treatment”, found the study. Experts say India should focus on early detection of cancer; treatment costs and survival rates are better when cancer is treated in early stages.
Economic cost
As in 2019
Cancer is killing not just Indians but India's economy too, February 4, 2020: The Times of India
From: Cancer is killing not just Indians but India's economy too, February 4, 2020: The Times of India

From: Cancer is killing not just Indians but India's economy too, February 4, 2020: The Times of India
DEADLY DISEASE
This year, more than 17 lakh Indians will be diagnosed with various forms of cancer while more than 8 lakh will not live to see 2021 — according to the Indian Council of Medical Research (ICMR). In 2018, the disease led to nearly 7 lakh deaths. India already has 22.5 lakh people afflicted with cancer and the disease is the second most common cause of death after heart disease in India — responsible for 8.3% of all deaths, according to a joint ICMR-health ministry study in 2016. This was double its contribution to fatalities in 1990. According to the WHO, India's death rate due to cancer is 79 per 100,000 deaths — while the number of deaths due to cancer in India are 6% of worldwide cancer-related deaths.
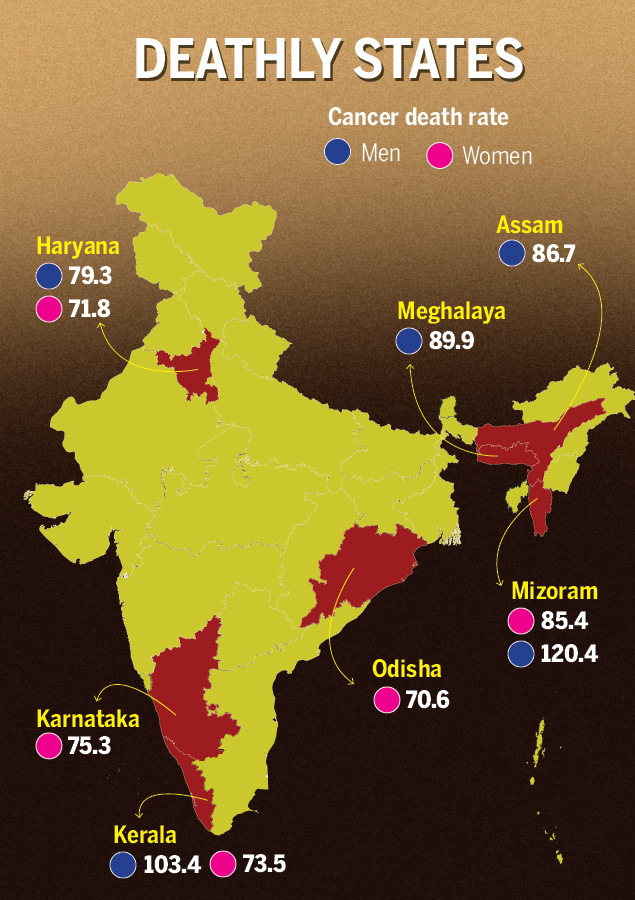
KERALA HAS MOST CANCER CASES
The highest number of cancer cases are in Kerala, followed by Mizoram, Haryana, Delhi and Karnataka, while Bihar has the least. In 2016, cancer incidence rate in India was 106.6 per 1 lakh people, while Kerala had a rate of 135.3 per 1 lakh people. In terms of the death rate for both sexes due to cancer, Mizoram topped the list, followed by Kerala, Assam and Haryana, according to the Lancet report, ‘The burden of cancers and their variations across the states of India: Global burden of disease study 1990-2016’.
Dr A Nandakumar, director, National Centre for Disease Informatics and Research, Indian Council of Medical Research (ICMR), said Kerala has a slightly older population compared to the rest of the country and this could be reason for high incidence. “If you take the proportion of people above the age of 65 in Kerala, which is the age during which people are more prone to get cancer, it is high compared to the rest of India."
CERVICAL CANCER KILLED 60,000 INDIAN WOMEN
Overall, the incidence of cancer as well as the death rate among men is higher than women. However, breast cancer cases have seen an alarming rise over the past few years — nearly 60% of patients with breast cancer are diagnosed in advanced stages. It's the most common cancer in women in India, accounting for about a quarter of all cancer cases in women in Indian cities.
Also, in certain cancers, Indian women are more at risk than their peers elsewhere. In 2018, for instance, India recorded the highest number of deaths of women due to cervical cancer, with 60,000 women succumbing to the disease — which means that every 8 minutes and 46 seconds, an Indian woman died due to cervical cancer. It is the eighth leading type of cancer in India, after cancers of the stomach, breast, lung, lip & oral cavity, pharynx, colon & rectum and leukaemia.
COLON AND RECTUM CANCERS ON THE RISE
Anal, colon and rectum cancer cases, the sixth leading type of cancer, have also gone up in recent years, particularly in people below 30 years, thanks to the increasing use of mobile phones in the toilet, erratic lifestyle, stress and an unhealthy diet. Dr Arshad Ahmad, professor in department of oncology and expert in anorectal surgery, said: “Use of mobile phone in toilet diverts attention from defecation. This disturbs bowel movement leading to constipation which, if prolonged, turns chronic and causes haemorrhoid – a swollen vein or group of veins around anus. Sometimes, it causes bleeding. If constipation persists for 4-5 years, accumulation of bacteria may also lead to anorectal cancer.”
“Five years ago, we used to get 40-45 patients of anorectal cancer in a month and only 3-4 were below 30 years. But now, out of 40-45 anorectal cancer patients, 25 are below 30 years. In young patients, common factor for cancer is chronic constipation caused by excessive intake of low-fibre junk food, genetic disorders and use of mobile phones in toilets,” he added.
THE FINANCIAL COST Studies have pegged the average cost of cancer therapy per household at around Rs 37,000, that in no way is reflective of the actual cost incurred — which will be substantially more due to non-medical expenses. Out-of-pocket hospitalisation expenditure for cancer treatment is 2.5 times of the overall average hospitalisation expenditure — forcing 60% of the households to resort to borrowings and another 32% to seek financial aid from relatives and friends.
As for what it cost the country, a study by European Short Term Scientific Mission found that India lost 0.36% of its GDP, amounting to $6.7 billion, due to productivity losses from cancer, second only to South Africa. While the cost per death of productivity lost in India was a little under $20,000, lip and oral cancers dominated total productivity losses in the country — at an alarming $740 million — due to the rampant use of tobacco among Indians. A combination of tobacco control, alcohol control, vaccinations programmes, cancer screening and affordable healthcare is essential, not just for Indians' health but also for India's economy.
Hospitals
National Cancer Institute (NCI), Jhajjar
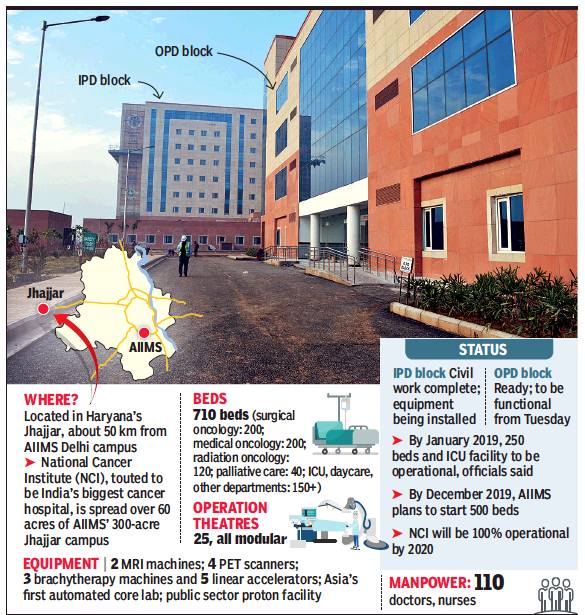
From: DurgeshNandan Jha, Country’s largest cancer hospital comes up in NCR, December 18, 2018: The Times of India
India’s largest cancer hospital — the National Cancer Institute (NCI) in Jhajjar in Haryana- commenced OPD services.
Civil work and installation of basic equipment in the hospital’s OPD block is complete and, on Monday, a day before the commencement of OPD services, the staff could be seen giving finishing touches for a smooth start of what is being touted as India’s largest public funded hospital project to come up in decades. It is being built at a cost of Rs 2035 crore.
Dr Randeep Guleria, director of AIIMS which is tasked with running the hospital, told TOI said civil work of 710-bedded hospital project is complete.
“We are doing soft launch of OPD services on Monday. By mid-January, indoor admissions will also be opened to public in phased manner,” he said. NCI will be started in three phases. In the first phase, which is likely to kickoff from January to March 2019, OPD services and 250 beds will be available.
By December 2019, indoor admission will be increased up to 500 beds and then in another one year plans are afoot to make it fully operational.
NCI will take the load off AIIMS’ existing cancer hospital which sees 1,300 patients daily. Only about 400 get treatment due to lack of facilities, say doctors.
Jhajjar campus is situated about 50 kilometers away from main AIIMS, but the officials involved with NCI said they plan to use technology for integration of services between the two campuses. For example, unique identity issued to patients will be the same for both centers. “For phase I, our manpower requirement is of 634 doctors, nurses and technicians. Of this, 110 are already on board and more staff are being hired,” officials said.
NCI is being headed by Dr G K Rath who is also the chief of Institute Rotary Cancer hospital at AIIMS. Sources said two linear accelerators — device used for external radiation — have been purchased by NCI at a cost of Rs 48 crore, in addition to CT scan and x-ray machines. A state-of-the-art lab that can process 60,000 sample daily is also ready. Once fully-operation, NCI will act as the nodal institution for all activities related to cancer care in the country.
Incidence of cancer
1990-2016, Lancet: rate static, but late detection> high mortality
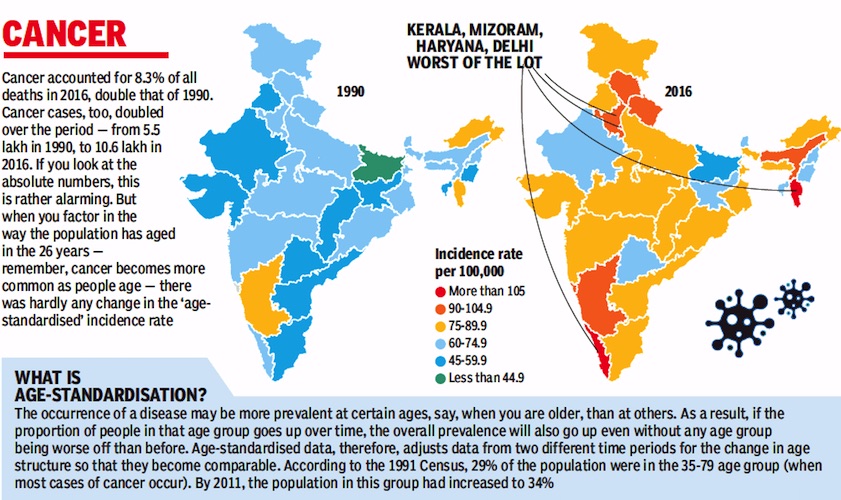
From: September 13, 2018: The Times of India
Study: Mortality High Due To Late Detection
Here’s a piece of information you may find hard to believe. A study undertaken by top researchers from Indian medical institutions has revealed that ageadjusted incidence of most common cancers, except breast cancer, has remained static in India over the last 26 years from 1990 to 2016.
While the actual incidence has gone up, it is almost entirely because of a change in the age structure of our population. People are living longer and that’s why diseases that affect relatively older people, for example cancer, show a greater prevalence.
According to a study published in The Lancet, incidence of cancer, except for cervical cancer, is much lower in India, excluding Mizoram, than in countries that can be said to be in a similar epidemiological transition, for example Brazil, Russia, China and South Africa.
Sadly, mortality rates due to cancer remain high, which could be reflective of poor access to early detection and curative services and the lack of affordability.
At present, doctors say survival rate for most cancers stagnates at 20% to 30% because a majority of the patients come to them when the disease is already in the advanced or III and IV stages.
“If cancer is detected early, 80% patients can be cured of the disease,” Dr GK Rath, chief of AIIMS cancer centre, told TOI.
The leading types of cancer among both sexes in India in 2016, as per the study, were stomach cancer (9%), breast cancer (8.2%), lung cancer
(7.5%), lip and oral cavity cancer (7.2%), pharynx cancer other than nasopharynx
(6.8%), colon and rectum cancer (5.8%), leukaemia (5.2%) and cervical cancer (5.2%).
Over the 26-year period, researchers said, the agestandardised rate of breast cancer in women has increased by 39.1%, with increase observed in every state. The age-standardised rate of cervical cancer, on the other hand, has decreased substantially by 39.7% in India from 1990 to 2016.
Professor Rajesh Dikshit of Tata Memorial Centre, Mumbai, said rising abdominal obesity, late age of child bearing, high use of oral contraceptives and genetic susceptibility are key reasons for higher incidence of breast cancer. “Cervical cancer cases are declining due to improvement in genital hygiene,” he added.
Lung cancer has been identified as the second most common cause of cancer among men in 2016, affecting 67,000 people. Tobacco use and air pollution were the leading risk factors for lung cancer-related morbidity and mortality.
Commenting on Lancet’s fndings on non-communicable diseases in India, Dr Balram Bhargava, director general of ICMR, said they emphasised the “need for prevention and management of major NCDs to receive as much policy attention as reduction of still high burden of communicable and childhood diseases”.
He added that the government’s plans of establishing 1.5 lakh health and wellness centres across India to provide comprehensive primary healthcare services would help deal with NCDs and injuries along with communicable diseases, as part of the Ayushman Bharat scheme.
1990 – 2019
DurgeshNandan Jha, Sep 5, 2023: The Times of India
New Delhi : There has been a 79% increase in cases of cancer among those in the under-50 age bracket globally in the past three decades, a study published in the British Medical Journal (Oncology) has found.
The number of such patients went up to 3.82 million in 2019 from 1.82 million in 1990.
Researchers found that the resultant deaths increased by 28% during the corresponding period.
The study is based on an analysis of data from the 2019 report of Global Burden of Disease covering 29 types of cancer in 204 countries and regions, including India.
Dr Devi Shetty, chairman of Narayana Health, said in creased awareness and availability of diagnostic tools is a key factor for rise in reported incidence of cancer in countries like India. However, he added the role of environmental factors behind the increase in cases could not be discounted.
Details
DurgeshNandan Jha , Sep 5, 2023: The Times of India
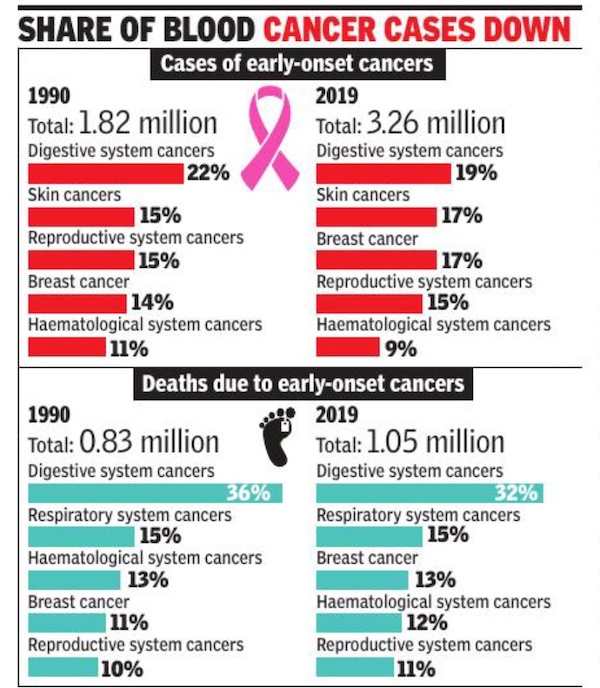
From: DurgeshNandan Jha , Sep 5, 2023: The Times of India
New Delhi : In the BMJ (Oncology) study, researchers found that breast cancer accounted for the highest number of early-onset cases in the under-50 age group in 2019, and cancers of the windpipe (nasopharynx) and prostate rose the fastest since 1990. Early onset windpipe and prostate cancers rose annually at an estimated 2.28% and 2.23% respectively between 1990 and 2019. At the other end of the spectrum, early onset liver cancer fell by an estimated 2.88%.
“Introduction of Hepatitis B vaccination in the universal immunisation programme has played an important role in reduction of liver cancer. But I feel that the gains made thereof may get undone due to a rise in incidence of non-alcoholic fatty liver disease that can lead to liver cancer,” said Dr Randhir Sud, chairman of Medanta Institute of digestive and hepatobiliary sciences. He said cancers of the digestive systems have also gone up. Based on the observed trends for the past three decades, the researchers estimated that the global number of new early onset cancer cases and associated deaths could rise by a further 31% and 21%, respectively by 2030, with those in their 40s the most at risk.
Genetic factors are likely to have a role but researchers say diets high in red meat and salt, and low in fruit and milk; alcohol consumption; and to bacco use are the main risk factors underlying the most common cancers among the under 50s.
“Prevention and early detection measures are urgently required, along with identifying optimal treatment strategies for early-onset cancers, which should include a holistic approach addressing the unique supportive care needs of younger patients,” they said. In2022, India recorded approximately 14.6 lakh cancer cases. By 2025, this number is projected to touch 15.7lakh.
1990-2023
DurgeshNandan Jha, Sep 29, 2025: The Times of India
New Delhi : The incidence of cancer in India has gone up by 26%, from 84.8 per 1 lakh population in 1990 to 107.2 in 2023, according to a new study. Published in The Lancet, it shows deaths due to cancer increased by 21% during this period, despite advances in treatment.
In comparison, both incidence and mortality have declined significantly in US and China over the 33-year period. The reason behind this is strong tobacco control, universal vaccination and organised screening in these two countries, Dr Abhishek Shankar, radiation-oncologist at AIIMS Delhi, said.
India, he added, continues to fare poorly on both counts because of persisting risk factors such as high use of tobacco, obesity and infections, coupled with limited access to early detection.
Study links 4.3m cancer deaths in 2023 to modifiable risk factors
Evidence-based strategies like HPV and Hepatitis-B vaccination, mammography, lung cancer screening with low-dose CT, and colonoscopy screening, and timely treatment remain uneven or inadequate.
For India to reverse its trajectory, we must urgently strengthen risk prevention strategies, expand evidencebased screening programmes and integrate cancer care into its universal health coverage agenda,” Shankar said.
The study’s lead author Dr Lisa Force from the Institute for Health Metrics and Evaluation (IHME), University of Washington, said, “Cancer remains an important contributor to disease burden globally and our study highlights how it is anticipated to grow substantially over the coming decades, with disproportionate growth in countries with limited resources.”
She added that despite the clear need for action, cancer control policies and implementation remain underprioritised in global health, and there is insufficient funding to address this challenge in many settings.
The study shows cancer incidence has declined by 19% and 20% in China and the US, respectively, between 1990 and 2023, while their mortality rates attributable to cancer has also seen a robust decline — 43% decline in mortality due to cancer in China and 33% in the US.
The study estimates that 42% (4.3 million) of the estimated 10.4 million cancer deaths in 2023 were attributable to 44 potentially modifiable risk factors — presenting an opportunity for action.
“Behavioural risk factors contributed to the most cancer deaths across all country income levels in 2023, especially tobacco use which contributed to 21% of cancer deaths globally. Tobacco was the leading risk factor in all country income levels except low-income countries, where the leading risk factor was unsafe sex (linked to 12.5% of all cancer deaths),” the study said.
A parliamentary committee report tabled in 2023 suggested raising taxes on tobacco products in India to make them less affordable.
“Committee recommends the ministry (health) to pursue with the department of revenue to expedite the decision on raising taxes on tobacco products,” it said.
It also stressed upon the need to link the PopulationBased Cancer Registry to Ayushman Bharat Digital Mission to get real time data on cancer patients.
The mission is a key health initiative by the govt which aims at providing digital health IDs for all Indian citizens to help hospitals, insurance firms, and citizens access health records electronically when required.
Most cancer cases in India are detected in late stages leading to poor prognosis.
The parliamentary committee suggested that the issue of screening for cancer should be taken up at ‘Jan Aandolan Pace’, a mass movement to fight against cancer by timely screening.
“A day in a month may be fixed for cancer screening on the lines of reproductive and child health,” the parliamentary committee suggested.
2012: How geography, soil, water influence the incidence
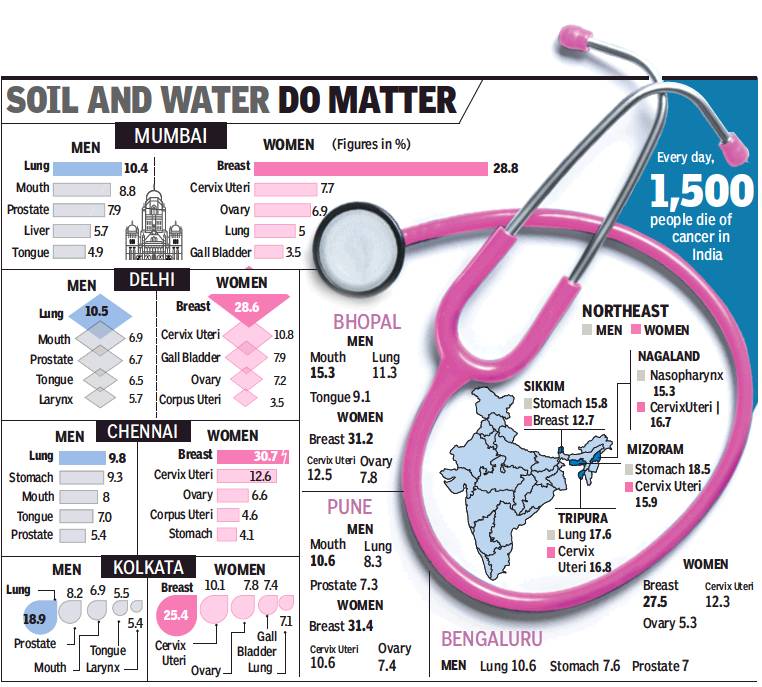
From: Pushpa Narayan & Prithvijit Mitra, Not lifestyle alone, geography too plays vital role in mapping of cancer cases, January 15, 2018: The Times of India
2,000 New Cases A Day In India, 17.3 Lakh Expected By 2020
Over two decades back, doctors at Tata Memorial Hospital, Mumbai, noticed that most gall bladder cancer patients were from the Gangetic belt states of Bihar, Uttar Pradesh or West Bengal. This led to a series of studies that found high concentration of heavy metals in the soil and ground water in this belt — a likely factor for high incidence of gall bladder cancer.
It is now well known that the incidence of gall bladder cancer is highest in the country’s eastern side while south India registers the lowest.
Environment and lifestyle are among the leading risks. The incidence of lung cancer is registering a rise in metros, be it Bengaluru or Delhi. Women in urban India are more likely to get breast cancer than those in rural areas.
The Indian government’s Million Death Study released in 2012 for the first time showed that that the area an Indian lives in, his economic and educational status and religion contribute to the malady’s outcome. A youngster from India’s northeast is four times more likely to develop and succumb to cancer than one from Bihar.
“There is growing evidence that environment and lifestyle can cause cancer in younger people as well,” said former director-general of ICMR, Dr Vishwa Mohan Katoch. “While some cancers are common, others are specific to a region,” he said, adding that in the Gangetic plains the risk of gall bladder cancer is very high due to polluted water, sediments in water and high consumption of animal protein and fish.
Every day, 1,500 people die of cancer in India, making it the second most common cause of death in India after cardiovascular disease. And nearly 2,000 new cancer cases are detected in the country daily, according to National Institute of Cancer Prevention and Research. Projections put the number of new cases by 2020 at 17.3 lakh.
In eastern India, rise in tobacco use has led to an increase in lung cancer among men, and rapid changes in food habits have made women more vulnerable to breast cancer, said Kolkata-based oncologist Gautam Mukhopadhyay.
Common cancers in the north-east are oesophagus, stomach and hypopharynx. Registries in the north-east have also recorded the country’s highest incidence of nasopharynx and gall bladder in Nagaland and Kamrupin Assam.
In Bengaluru and Chennai more than a quarter of the total number of cancers in women are of the breast. Bengalurubased Dr PP Bapsy said mass screening is most important to detect cancer early. “We need low cost, accessible treatment,” Dr Bapsy said.
Most oncologists insist that lifestyle changes will by itself bring down incidence. “By some magic, if everyone stopped using tobacco in India, we will have at 50% lesser cancer cases,” said Dr Rakesh Jalali, medical director of Apollo Proton Cancer Centre.
2012, statistics

The top five cancers among Indian men
From: Shimona Kanwar, Cancer hits more women in India than men, but more men die of it, January 10, 2018: The Times of India
Docs Say Women Get Greater Medical Attention So Detection Is Early
Estrogen, the female sex hormone that shields young women against cardiovascular diseases, plays a role in her battle with cancer as well. It not only increases her chances of getting the disease, but also increases her chances of survival, say doctors.
Statistics prove this. The World Health Organisation-developed statistical tool called Globocan 2012 shows that the Big C has afflicted more Indian women than men. But more Indian men died due to cancer than women, said the World Cancer Report 2014.
Doctors in Chandigarh’s Postgraduate Institute of Medical Education and Research (PGI-MER) surmise women are subjected to more medical attention in their lifespan, allowing cancers to be picked at an early stage and hence improving their life expectancy.
In all, 5.37 lakh Indian women got cancer in 2012 as against 4.77 lakh men, said the World Cancer Report. But 75% of the men affected with cancer have low life expectancy, while the mortality rate of cancer in women is 60%. In 2012, 3.56 lakh men died of the disease in comparison to 3.26 lakh women.
Among all cancers in both sexes, the incidence of breast cancer is highest at 1,44,937, while the cervix uteri is the second most frequently occurring cancer with an incidence of 1,22,844. The third most common cancer is of the lip and oral cavity with 53,842 men affected.
This gender bias in cancer is noticeable. Dr Rakesh Kapoor, department of radiotherapy at the Postgraduate Institute of Medical Education and Research, Chandigarh, said, "Women are subjected to more medical attention in their lifespan as compared to men. From antenatal check-up, menopause problems and menstrual disorder, women get investigated and, by default, screened for cancer. Therefore, cancers are picked up at an earlier stage and the mortality is less." He said most national policies for screening are directed more towards cancers that hit women such as breast cancer and cervix cancer, as they are noninvasive. "Also, men have prolonged exposure to lifestyle risk factors that cause cancer such as tobacco use, substance abuse and alcohol consumption," Dr Kapoor added.
Why is cancer mortality higher among men? Doctors say this could be because the lung and oral cavity cancers that are the leading cancers among men are usually detected at a late stage. "Around 95% of these cancers are due to tobacco consumption, and 40% of all the cancers in India are due to tobacco abuse. The mortality in such cancer cases is high as it is difficult to detect these cancers. We come across patients during an advanced stage of the disease, and thus they are tough to treat," said Dr Ravi Mehrotra, director of the ICMRaffiliated National Institute of Cancer Prevention and Research.
Incidentally, the latest Globocan report says that globally the overall age standardized cancer incidence rate is almost 25% higher in men than in women.
The World Cancer Report estimates that of the 1,589,925 lung cancer deaths worldwide in 2012, 30.90% were of women and 69.10% of men. "Breast cancer is detected early, particularly in the western world. There is no screening of cancers in men. So we have this pattern of high incidence of cancer among women mainly due to screening," said Dr Rajesh Dixit, professor of epidemiology at the Centre for Cancer Epidemiology, Tata Memorial Centre, Mumbai.
As per the latest cancer registry of ICMR, cancer of the breast, with an estimated 1.5 lakh (over 10 per cent of all cancers) new cases during 2016, is the number one cancer overall.
2012-18 statistics
In 6 yrs, oral cancer cases rise by 114% in India: Study, November 16, 2018: The Times of India

From: In 6 yrs, oral cancer cases rise by 114% in India: Study, November 16, 2018: The Times of India
The number of cancer cases countrywide has gone up in the last six years by 15.7%. Data shared by Indian Council of Medical Research’s National Institute of Cancer Prevention and Research showed that 11.5 lakh cancer cases were reported across the country in 2018, as against 10 lakh in 2012.
Experts from Tata Memorial Hospital (Parel) said the increase was not alarming as it can be explained with factors such as increased population and better diagnostic techniques. As per the new data, cancer-related deaths also increased by 12%. While 7 lakh Indians died of cancerrelated complications in 2012, the number increased to 7.8 lakh this year.
ICMR cancer centre director Dr Ravi Mehrotra said lip and oral cavity cancers increased by a whopping 114% in the six-year period. Breast cancer, emerging as a disease linked to urban lifestyle, increased by almost 11%, from 1.4 lakh in 2012 to 1.6 lakh in 2018.
These numbers are estimates provided by web-based Globocan programme that was developed by International Agency for Research on Cancer and World Health Organisation. IARC released the 2018 estimates recently.
The silver lining in the estimates is the sharp decrease in cases of cervical cancer, which until a decade back was the No. 1 cancer among Indian women. Globocan data showed a 21% fall in cervical cancer cases, from 1.23 lakh in 2012 to 96 in 2018.
Dr Mehrotra said, “An increase in awareness, better screening and treatment facilities, later age of marriage, fewer pregnancies and improved hygiene leading to fewer infections are some key factors contributing to this decline in cervical cancer cases.”
Dr Rajesh Dikshit, who heads Tata Memorial Centre’s epidemiology department said the incidence of cervical cancer had started decreasing in Mumbai many years back. “A decade back, the incidence in Mumbai was 17 cases for every 100,000 population, but the incidence has now dropped to 8 per 100,000 in Mumbai,” he said.
ICMR officials said as 18% of the world’s population lived in India, it was important to understand the disease burden of cancer in every state of India. ICMR released an elaborate state-wise data of cancer along with medical journal, ‘The Lancet’, last month.
2014: Incidence
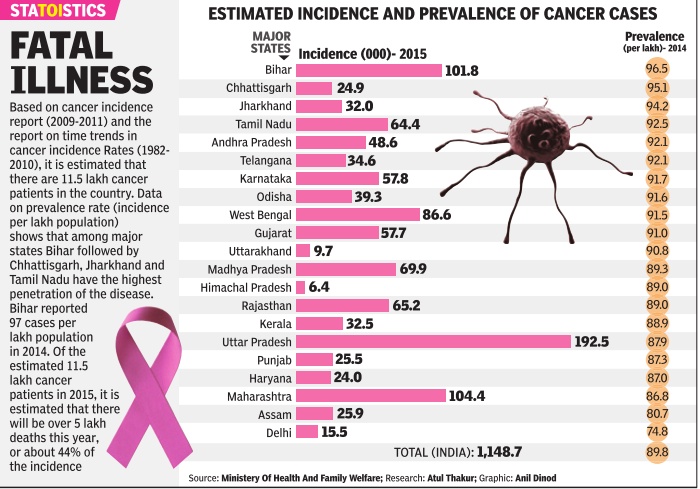
See graphic, 'Estimated incidence and prevalence of cancer cases, state-wise, 2014'
2016> 2018: state-wise
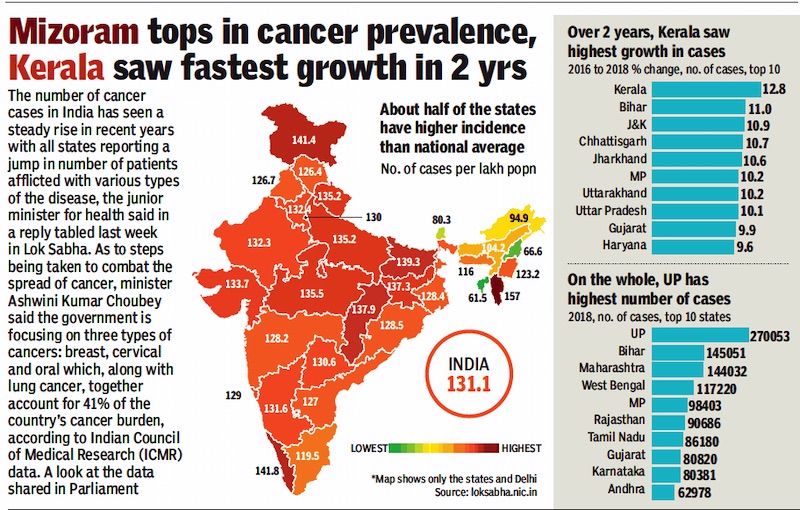
From: Nov 25, 2019: The Times of India
See graphic:
2016> 2018: The state-wise incidence of cancer in India
2016-2019
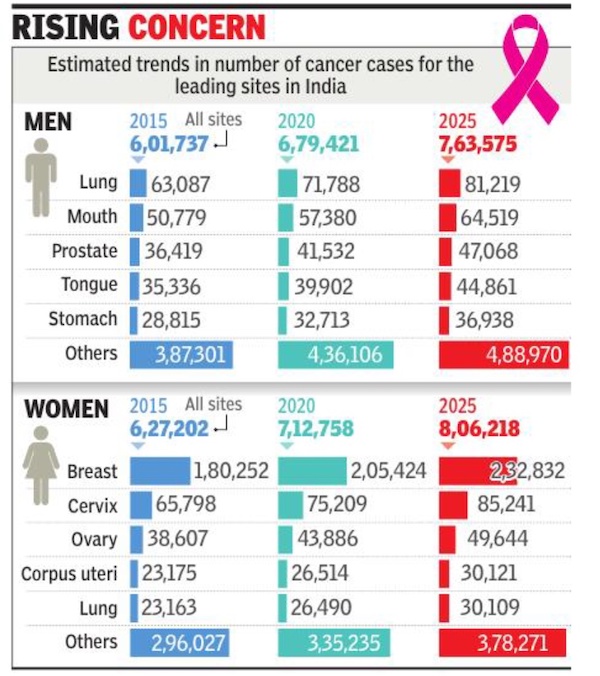
Cancer cases rise 10% in 4 yrs to 13.9L, August 19, 2020: The Times of India

From: Cancer cases rise 10% in 4 yrs to 13.9L, August 19, 2020: The Times of India
Cancer cases have risen by about 10% over the last four years in India to reach 13.9 lakh in 2020 and could touch 15.7 lakh by 2025. As per the National Cancer Registry Programme Report 2020, cases were estimated at 12.6 lakh in 2016 and 13.6 lakh in 2019.
The estimates are based on collation of data for the period between 2012 and 2016 and extrapolations from those trends. Already, cancer impacts more women than men in terms of overall numbers going by the data from 2016 and it is projected that this will continue in the years to come.
‘Breast, lung & mouth cancers to be common types by 2025’
The report released by the Indian Council of Medical Research and the National Centre for Disease Informatics & Research, Bengaluru, projects that the number of male cancer cases this year would be 6.8 lakh while the number of women impacted is pitched at 7.1 lakh. The numbers are projected to reach 7.6 lakh for men and 8.1 lakh for women in 2025. Data related to cancer was collected from 28 population-based cancer registries and 58 hospital-based cancer registries.
Breast cancer (2.4 lakh) is expected to be the most common cancer in 2025 followed by lung (1.1 lakh) and mouth (90,000) cancers. Tobacco-related cancers are estimated to constitute 27% of all cancers in India. As per the report, in 2020, tobacco-related cancers are estimated to contribute 3.7 lakh (27%) of the total cancer burden. Among women, breast cancers are estimated to contribute 2 lakh (14.8%) while cervix cancer is estimated to contribute 75,000 (5.4%). For men and women put together, cancers of the gastrointestinal tract are estimated to contribute 2.7 lakh (19.7%) of the total cancer burden.
Cancers related to the use of any form of tobacco were highest in the northeastern region of India. Cancers of the lung, mouth, stomach and oesophagus were the most common cancers among men.
2018
Sushmi Dey, Nov 3, 2019: The Times of India

From: Sushmi Dey , Nov 3, 2019: The Times of India
The states which recorded the most cases of common cancer in 2018 — Gujarat, Karnataka, Maharashtra, Telangana and West Bengal — also recorded a significant jump in cases as compared to the previous year, according to National Health Profile, 2019 data. For instance, the number of people diagnosed with common cancer in Gujarat jumped from 3,939 in 2017 to 72,169 in 2018, recording 68,230 new cases, whereas the number of those visiting clinics increased by only 24%.
Even states like Andhra Pradesh and UP, where the numbers of diagnosed cases were comparatively less, reported a significant jump in 2018 as compared to the previous year.
“Consumption of tobacco products is a major factor contributing significantly to oral cancers, especially when it is coupled with alcohol, the risk and incidence is much higher. Besides, a sedentary lifestyle and rising rate of obesity are causing a rapid increase in all kind of cancers,” says Dr Harpreet Singh, senior consultant oncologist at Action Cancer Hospital.
Doctors also strongly recommend breastfeeding to counter the incidence of breast cancer.
2018: an increase
Sushmi Dey, Dec 15, 2019 Times of India
Cancer care accounted for 34% of all tertiary claims submitted under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PMJAY) in the first 11 months since its launch in September 2018, a data analysis by the National Health Authority shows, indicating a rising incidence of cancer even as the insurance scheme makes treatment accessible to many.
Women accounted for higher number of claim submissions in all age-categories, with the highest numbers in the age group of 45-50 years. While ovary, breast, cervix and radical hysterectomy were common among women, men who sought oncology services under the scheme either came for stage three of palliative treatment or with colon rectum and head and neck cancers.
“The analysis presents highlights of broad trends of the oncology services utilisation and demand-supply scenario for the first 11 months under the scheme. This data is important as it can be used not only to align services and coverage under the scheme but also for better policy formation,” NHA chief executive Indu Bhushan told TOI.
PMJAY is the government-funded health insurance scheme that aims to provide free health cover of Rs 5 lakh annually to more than 10.74 crore deprived families.
The scheme offers 150 oncology packages.
The analysis of utilisation of oncology services under the scheme also highlights state-wise variation.
Tamil Nadu and Maharashtra together generated over 60% of all oncology claims. This is probably because Tata Memorial Hospital and Research Centre in Mumbai, followed by Government Super Speciality Radiology, Omandur in Tamil Nadu were the top hospitals catering to claims under oncology.
Migration for cancer care is most prominent in Madhya Pradesh followed by Uttar Pradesh, Bihar, Jharkhand and Maharashtra. These states accounted for 80% of the beneficiary movement for cancer care services.
To address the disparity and establish uniform standards for prevention, diagnosis and treatment of cancer across the country, NHA— the implementing agency for the scheme— has partnered with National Cancer Grid.
The Grid helps in linking doctors and specialists across the country to enable standard care across the country while saving patients the hassle of travelling long distances to seek treatment. The analysis also pointed at the higher utilisation of medical oncology packages, followed by radiation and surgical oncology. Over 80% of the total oncology claims were of medical oncology, whereas radiation oncology accounted for 13.8% and surgical oncology was 3.3%. Paediatric cancer accounted for 2.7% of total claims submitted for oncology services.
Experts say this could be because most cancer cases in the country are diagnosed at a late stage and therefore, such patients are generally treated with palliative therapy part of medical oncology.
Overall, majority (72%) of the claims were from private hospitals, except in six states or UTs which includes Andaman and Nicobar, Arunachal Pradesh, Chandigarh, Kerala, Mizoram and Sikkim. These states generated no oncology claims at private hospitals.
The analysis points at differences in waiting time, distance, equipment’s, availability of specialisation and multifaceted cancer centers as some of the possible reasons for the gap between utilisation of services in public and private sector.
2018: 1/10 Indians will develop cancer; 1/15 Indians will die of cancer
Sushmi Dey February 5, 2020: The Times of India

From: Sushmi Dey February 5, 2020: The Times of India
‘1 in 10 Indians to get cancer in lifetime’ WHO Says Disease Will Kill 1 In 15 Indians; World May See 60% Rise In Cases In 20 Yrs
One in 10 Indian will develop cancer during their life-time and one in 15 Indians will die of cancer, says the World Cancer Report released by World Health organisation (WHO) which has pointed out “socio-economic inequalities” as a major cause for the rapidly increasing burden of the disease in the country.
Lower socio-economic status is associated with oral and cervical cancer while urbanisation, improvement in education and increasing disposable income with higher overall socio-economic status are associated with an increasing risk of breast and colorectal cancer cases.
India had an estimated 1.16 million new cancer cases and around 7.84 lakh cancer deaths in 2018. The six most common cancer types are breast, oral, cervical, lung, stomach, and colorectal cancer. Together, these accounted for almost half (49%) of all new cancer cases.
The report shows over 90% of patients with oral cancer have lower socio-economic status in India because nonawareness about harms of tobacco use is common among these people. Similarly, cervical cancer disproportionately affects women with lower socio-economic status, who have limited access to public health services. India accounts for about one fifth of the global burden of cervical cancer, despite decreasing incidence in several regions of the country.
On the contrary, incidence of colorectal and breast cancer is increasing in the most developed states in India and in urban population. Experts say improvement in socio-economic status and urbanisation have led to sedentary lifestyle, more stress, less of breast-feeding, poor eating habits and higher prevalence of obesity.
The report also shows households with high socio-economic status spend less on cereals, millets and vegetables and more on processed and dairy products, meat, eggs and fish. It suggests “highly focused and tailored public health interventions” to target different socio-economic groups to reduce disparities in cancer prevention.
The UN agency warned that if current trends continue, the world will see a 60% increase in cancer cases over the next two decades with the biggest increase (an estimated 81%) in new cases in low and middle-income countries.
WHO pointed specifically at low socio-economic status, consumption of tobacco products and poor child and maternal health along with limited health resources for combating infectious diseases as reasons for the rapidly increasing cancer burden.
“This is a wake-up call to tackle the unacceptable inequalities between cancer services in rich and poor countries,” said Ren Minghui, WHO assistant director-general for universal health coverage. “If people have access to primary care and referral systems, cancer can be detected early, treated effectively and cured. Cancer should not be a death sentence for anyone, anywhere.”
2015- 20, incidence and likelihood
DurgeshNandan Jha, Dec 17, 2022: The Times of India
From: DurgeshNandan Jha, Dec 17, 2022: The Times of India
New Delhi : One in every nine persons in India is at risk of developing cancer in his or her lifetime, reveals a study carried out by the ICMR-National Centre for Disease Informatics and Research (NCDIR). It is based on a statistical analysis of the number of new cases of the disease being reported in the country vis-àvis the number of individuals in the population at risk.
According to the study, which has been published in the Indian Journal of Medical Research (IJMR), one in every 67 men ia at risk of developing lung cancer and one in 29 women is at risk of developing breast cancer in their lifetime (0-74 years). It is estimated that 14. 6 lakh people were affected by cancer in India in 2022. Lung and breast cancers were the leading sites of cancer in men and women, respectively. Among childhood (0-14 year) cancers, lymphoid leukaemia (boys: 29. 2% and girls: 24. 2%) was the leading site, the study suggests. “The incidence of cancer cases is estimated to increase by 12. 8% in 2025 as compared to 2020,” it adds.
Researchers say the increase in cancer cases was attributable to the changes in population dynamics and its growth. India, they add, is expected to see an increase in the older age (60+) population, and especially their proportion is expected to increase from 8. 6% in 2011 to 9. 7% in 2022.
“There would be changes in estimated cancer incidence, which depends upon the risk factors, improvement in case findings, introduction ofscreening programmes and cancer detection and diagnosis techniques,” researchers said. Estimated cancer cases and mortality due to it have increased in the country between 2020 and 2022, health minister Mansukh Mandaviya told Rajya Sabha.
The department of health and family welfare provides technical and financial support to states and Union Territories under the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) as part of the National Health Mission (NHM), based on the proposals received from the states and subject to the resource envelope, Mandaviya said in reply to a question.
Cancer is an integral part of NPCDCS, the minister said, adding that the programme focusses on strengthening infrastructure, human resource development, health promotion and awareness generation for cancer prevention, early diagnosis, management and referral to an appropriate level of healthcare facility for treatment.
Under NPCDCS, 707 district NCD clinics, 268 district daycare centres, and 5,541 community health centre NCD clinics have been set up. Setting up of National Cancer Institute at Jhajjar (Haryana) and second campus of Chittaranjan National Cancer Institute, Kolkata are also steps in this direction, the minister said.
Cancer cases lower than in West, yet death rate higher

From: India’s cancer cases far lower than those in West, yet death rate higher, January 18, 2018: The Times of India
See graphic:
Cancer rate per 100,000 population- How India compares with the rest of the countries
Poor Awareness, Social Stigma Reasons For Delayed Detection
India’s cancer graphs tell two distinct stories. The first holds out hope as India’s cancer incidence is far lower than developed nations such as Denmark and the US. If cancer strikes over 300 out of every 100,000 population in Denmark, the corresponding number in India hovers around 80. But the second Indian cancer story is worrisome: cancer manages to get the upper hand in almost 70% of cases in India. A study in medical journal, The Lancet, in 2014 indicated only 30% of India’s cancer patients survive for over five years.
So while India has lower cancer rates than many other countries, it has a high death rate. Check the World Health Organisation’s Globocan 2012 report’s analysis for breast cancer: only 1out every 5 or 6 women newly diagnosed with breast cancer died in the US, but corresponding figures in India stood at 1 out of every 2 patients.
Experts said early detection could go a long way in reducing the high death rate caused due to illiteracy, fear and taboos. “In India, almost 50% of all cancers are seen in late stages. This is the reason our death rate is higher than western countries,” said senior medical oncologist Shona Nag.
Maximum cancer patients succumb to lung, head and neck and breast cancers. “We lose almost 80% of all patients detected with lung cancer. The death rate due to breast cancer world over is 20%, but we lose over 50% of our breast cancer patients,” Nag said.
Almost 80% of cervical cancer patients are diagnosed in stage 3-4 in India, but the West has almost eradicated this cancer due to regular pap smear tests. Given India's population, it is impossible to scan everybody. “Self-breast exams and clinical exams involving community workers or ancillary health professionals are hence crucial,” she added.
Lack of awareness is the main cause for late detection. “In the western world, the culture is openness and they are more aware. Though we have facilities, we cannot reach out to such a huge population. Almost all cancers are detected at late stage in India mainly because of lack of awareness and social stigma,” said medical oncologist Anantbhushan Ranade.
Cancer surgeon Anupama Mane said, “We have women with 10cm lumps who come to us late because the lump didn’t hurt or cause pain so they did not think a check was needed.” Moreover, men don’t discuss women’s health. “So a blood stain or excessive bleeding is dismissed and not taken up as cause for worry,” Mane said. Early detection is key to reduce mortality.“It is important to diagnose cancer early because then you have a chance at curing it. The spread and extent of it make it harder to control,” said oncosurgeon Snita Sinukumar. Lack of a dedicated health care system is one of the big reasons for higher deaths. “Just like Aadhar, we need to make it compulsory to invest in one’s own healthcare,” Sinukumar added.
Rachel Chitra, Cancer-related claims rise 16% a yr, January 27, 2018: The Times of India

From: Rachel Chitra, Cancer-related claims rise 16% a yr, January 27, 2018: The Times of India
See graphic:
Increase in Cancer-related claims, from 2015-16 to 2016-17, according to gender and type of cancer
With cancer-related claims rising 15.5% year-on-year and an average of 14.5 lakh cases detected in India, growing incidents of breast cancer are alarming. Recent data with Bajaj Allianz shows that breast carcinoma contributes to around 24% of the total cancer hospitalisation claims.
Indian Council of Medical Research estimates that by 2020, India will see more than 17.3 lakh new cases of cancer and over 8.8 lakh deaths due to the disease. Data shows that breast and cervical cancer for women and lung and mouth cavity for men are most frequent.
In 2016-17, it was seen that blood and lymphatic cancer was the second most frequent, contributing 16% of the cancer claims. This category also saw a 26% rise in claims over the previous year. Digestive tract related cancer claims account for 16% of overall claims, which saw a surge of 22% year-overyear. Data revealed that men were more prone to bone, joints and skin cancer than women.
“In our experience, the average surgical treatment cost for cancer is around Rs 1,75,000 and and average medical treatment cost is Rs 75,000. Majority of cancer-related claims are in the 46-55 and 56-65 age band,” said Bhaskar Nerurkar, head-health administration team, Bajaj Allianz General. “There are claims for people as young as 30.”
Once a year, insurers advice that policyholders could go for preventive check-ups like mammography for breast cancer and PAP smear for cervical cancer, PSA (prostate specific antigen) for prostate cancer and Xrays for lung cancer. Many insurers offer such tests free-of-cost for their policyholders at affiliated scan centres.
“Due to steady rise in noncommunicable disease over the past few years along with rise in medical inflation, the treatment cost of cancer has definitely put a lot of stress on finance of an individual. Therefore, there is a strong need for individuals to look for a comprehensive critical illness policy, which covers not just cancer but also heart disease/cerebrovascular disease and others,” he added.
Lung cancer
Among non-smokers
Delhi: 60% of patients are non-smokers
The Times of India, Feb 04 2016
DurgeshNandan Jha
20% of Delhi's lung cancer patients non-smokers: Docs In what could be an alarming fallout of air pollution, top oncologists say they have noted a significant rise in lung cancer among non-smokers. Roughly one in every five persons diagnosed with the disease does not smoke.
Delhi Cancer Registry data shows lung cancer cases ta shows lung cancer cases have been increasing among women too -from 4.2 cases per 1,00,000 population in 2008 to 4.6 in 2010. DCR, which compiles data from all big hospitals in Delhi, is yet to release data beyond 2010.
While the data is based on cases in Delhi, doctors said it represents a wider trend because a significant number of cancer patients being treated in hospitals are from outside.
In 2013, the International Agency for Research on Cancer (IARC), the specialised cancer agency of the World Health Organisation (WHO), classified outdoor air pollution as carcinogenic. It issued a statement saying there was sufficient evidence that exposure to outdoor air pollution causes lung cancer and increases risk of bladder cancer.
Particulate Matter (PM), a major component of outdoor air pollution, was evaluated separately and also classified as carcinogenic by IARC the same year. “The predominant sources of outdoor air pollution are transportation, power generation, industrial and agricultural emissions, and residential heating and cooking,“ the IARC stated.
Lung cancer hits non-smoking Indians earlier than Westerners/ c.2020
July 12, 2024: The Times of India
From: July 12, 2024: The Times of India
Mumbai : A lung cancer patient in India is likely to be 10 years younger than a patient in the West and possibly someone who avoids smoking, a lifestyle factor associated with it.
This typical, though unique, profile of an Indian patient has emerged in a special review of lung cancer cases in Asia in The Lancet, one of the most widely read medical journals in the world. Studies have shown that lung cancer presents approximately a decade earlier in India as compared to Western countries, with a mean age at diagnosis of 54-70 years.
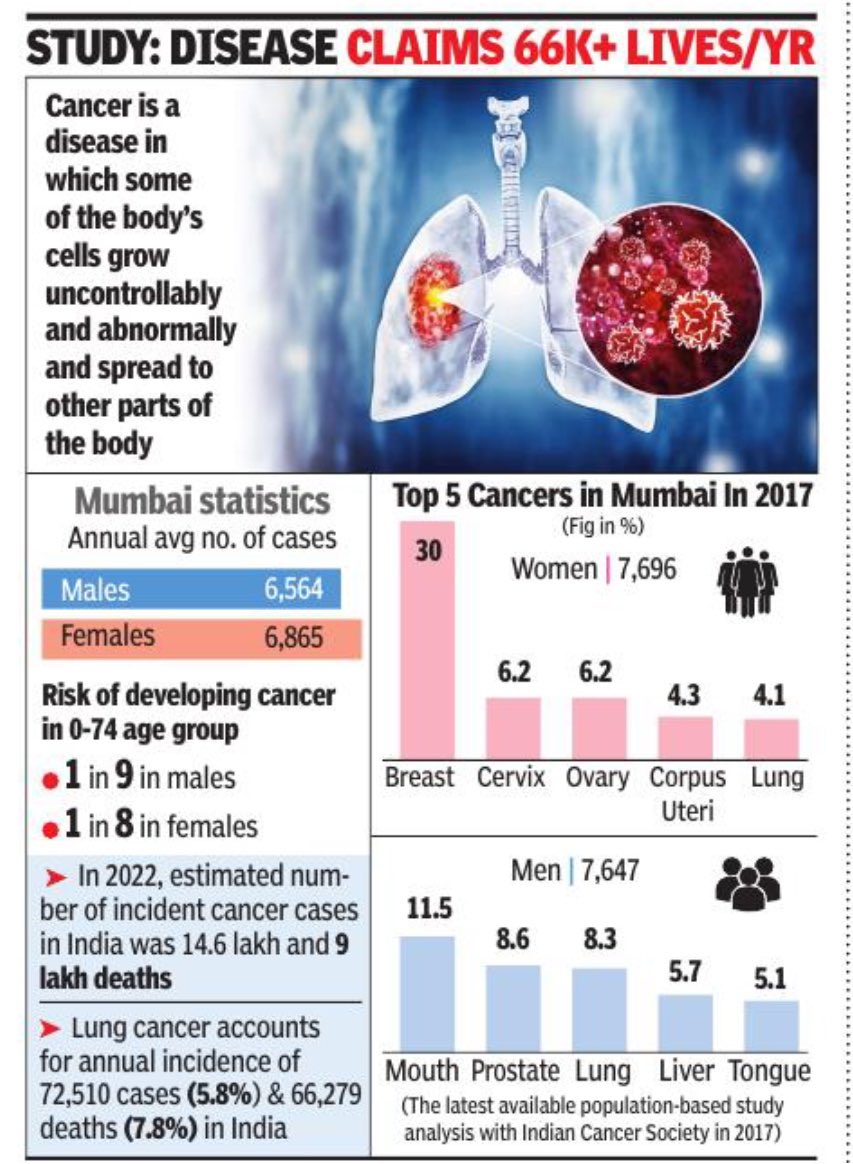
Written by a team of doctors, mainly from Tata Memorial Centre in Mumbai, the article, titled ‘Uniqueness of lung cancer in Southeast Asia’, said lung cancer was the third most commonly diagnosed cancer (18.5 lakh new cases or 7.8%) in this region in 2020, but it is the commonest cause of cancer mortality, causing 16.6 lakh or 10.9% deaths. The corresponding global figures are 22 lakh new cases (11.6%), causing 17 lakh deaths (18%). In India, lung cancer accounts for an annual incidence of 72,510 cases (5.8%) and 66,279 deaths (7.8%).
Highlighting the “uniqueness” of Indian patients, one of the authors, Dr Kumar Prabash from Tata Medical Centre’s medical oncology department, on Tuesday told TOIthat “over 50% of our lung cancer patients are non-smokers”.
The study said the important risk factors for lung cancer in non-smokers included air pollution (especially particulate matter PM2.5), occupational exposure to asbestos, chromium, cadmium, arsenic and coal as well as se- cond-hand smoke at home. Factors like genetic susceptibility, hormonal status, and pre-existing lung disease could also play a role in the rising lung cancer incidence in never-smokers.
Dr Prabash further said the proportion of cases here is lower than in the West. “The incidence rate of lung cancer in the US is 30 per 1,000, but it’s 6 per 1,000 in India. Given our huge population, however, even the 6% works out to a huge number of patients.”
Another uniqueness about India’s lung cancer pro- blem, he said, is the high incidence of TB. “Diagnosis often gets delayed because of TB as both conditions mimic each other.” In this regard, the authors said it’s not easy to get access to newer treatment modalities and molecules. “Most treatments are developed abroad, and importing them adds to the cost.” The biggest challenge is early identification and start of treatment. “Barely 5% of lung cancer patients seek help in time for surgical help. We need to increase this number to at least 20% like in the West,” Dr Prabash said.
Mortality rate
3 out of 5 in India succumb to cancer after diagnosis: ICMR/ 2022
DurgeshNandan Jha, February 26, 2025: The Times of India
New Delhi : Nearly three out of five people in India succumb following cancer diagnosis, Indian Council of Medical Research (ICMR) has claimed. The apex health research agency’s claim is based on an analysis of the estimates of incidence and m ortality of cancer from GLOBOCAN 2022 — an online database that provides cancer statistics for 185 countries.
India is one of the largest contributors to global cancer burden, ranking third in terms of new incidences. China ranks one in cancer incidence followed by the US.
According to the ICMR study, published in the journal ‘The Lancet Regional — Southeast Asia’, the incident to mortality percentage in India stands at approximately 65, which means that three out of five individuals would be expected to die if diagnosed with cancer. The incident to mortality percentages in China and the US stand at 50 and 23 respectively, according to the study. Children (0-14) and reproductive-age (15-49) individuals, ICMR says, have a 0.1%–2.3% chance of developing cancer and a 0.08%–1.3% chance of dying from it. However, the study adds, middleaged and geriatric individuals have a higher 8.3%–10.3% chance of developing cancer with a 5.5%–7.6% chance of dying from the disease.
Women bear a “disproportionate burden” with higher crude incidence (104.5 per 1,00,000 population) and crude mortality rate (64.2 per 1,00,000) compared to men (91.5 per 1,00,000 and 62.2 per 1,00,000), according to the study, which also says that trend analysis for past mortality patterns indicate cancer mortality rates in India are on the rise for last two decades.
Future projections show that cancer incidence and mortality will continue to rise in the coming years, with mortality rates expected to increase from 64.7 to 109.6 between 2022 and 2050, it s ays. ICMR warns India is poised to face formidable challenge in cancer control in coming years due to the transition of the current reproductive-age population (15-49 years) to middleaged (50-69) and geriatric (70+) groups. It has called for proactive measures to enhance early detection, access to quality care, and public health initiatives.
Chairperson of Max Institute of Cancer Care, Dr Harit Chaturvedi, said fight against cancer must be multipronged. “We need to createawareness on avoiding unhealthy eating and sedentary lifestyles that are linked to development of several noncommunicable diseases, including cancers,” he said. He added that diagnostic facilities and treatment for cancer need to be made accessible and affordable for early detection and improved outcome. Realising the challenge posed by the rising incidence and mortality caused by the disease, govt in the Union budget 2025-26 said it is planning to have daycare cancer centres in all 759 districts of the country where chemotherapy, essential medication and biopsy services will be made available. Top health ministry officials said these centres will also be utilised for screening high-risk individuals for common cancers.
Region-/ state-wise incidence
Arunachal Pradesh, Mizoram, NE/ 2020
August 19, 2021: The Times of India
Arunachal Pradesh’s Papum Pare district and Aizawl in Mizoram recorded the highest incidence of new cancer cases in the country among females and males respectively, as per a government report.
The report, released by the Indian Council of Medical Research (ICMR) and National Centre for Disease Informatics and Research (NCDIR), stated that Papum Pare district has 219.8 per one lakh cancer cases among females.
Mizoram’s capital Aizawl has 269.4 per one lakh cases among males, it said. Northeast India is the cancer capital of the country with the highest ageadjusted cancer incidence rates of newly diagnosed cancer cases, said Dr Kaling Jerang, the principal investigator of Population Based Cancer Registry (PBCR) at Bakin Pertin General Hospital in Pasighat.
The PBCR project under the ICMR-NCDIR, Bengaluru, has been studying the cancer trends under the National Cancer Registry Programme (NCRP), he said.
He hoped that the cancer data revealed by the project will be used by the government in policy-making decisions regarding cancer prevention, treatment and management. The estimated number of cancer cases in the northeast in 2020 was 50,317, among whom 27,503 were males and 22,814 females, the report said.
Oesophagus cancer was most prevalent in the region with cases 5,785 last year, it said. Oesophagus cancer will continue to be most prevalent in the northeast till at least 2025, the report predicted.
Breast and lung cancer are the next most common types of cancer found in the northeast, as per the report. There were 3,674 breast cancer cases in the region last year and 3,413 cases of lung cancer, it added.
The ICMR-NCDIR study further revealed that Papum Pare also recorded the steepest age adjusted incidence rate (AAR) for cancer of the stomach (males), liver (both genders), cervix uteri, ovary and thyroid.
Across northeast, oesophagus cancer (13.6%) is the highest among males, followed by lung cancer (10.9%) and stomach cancer (8.7%).
Among females, the breast is the leading cancer site (14.5%), followed by cervix uteri (12.2%) and gallbladder (7.1%), the report said. PTI
Statistics, year-wise
Extent and gender divide: 2012
Cancer strikes more Indian women, but kills more men
Malathy Iyer The Times of India Feb 04 2015 Mumbai
More Indian women than men are diagnosed with cancer every year. It is reflected in insurance statistics that show more women in our cities claim medical insurance for cancer treatment. Blame it on physiology or the stereotypical image of an Indian woman who chooses to ignore her symptoms for long, but fact is the Big C exhibits a clear gender divide.
But when it comes to cancer-related fatalities, the figures turn upside down: more men die of cancer annually than women.
In all, 5.37 lakh Indian women were diagnosed with cancer in 2012 as against 4.77 lakh men, according to the World Cancer Report. The same year, 3.56 lakh men died of the disease in comparison to 3.26 lakh women.
In the past four years, 62-65%of cancer-related insurance claims were for women while the figure for men was only 35-38%, according to data released by private insurance firm ICICI Lombard. The claims were more for cancers of the cervix and breast, which are, according to the Indian cancer registry, the leading cancer types among women.
The main reasons for the gender divide in cancer are hormones and habits. “Physiologically, women’s cells are exposed to more hormones and more hormonal fluctuations, leading to an increased susceptibility of cell dysplasia (abnormality),” said Dr Boman Dhabar, medical oncologist with Wockhardt Hospital in Mumbai Central.
He believes “oppression of Indian women” leads them to neglect their own health. “There are also socio-economic reasons such as lack of hygiene and toilets that lead to an increased incidence of cervical cancer,” said Dr Dhabar.
Dr Surendra Shastri, who heads the preventive oncology department of Tata Memorial Hospital, had another reason. “There is an increase in the incidence of lifestyle-related cancers, for example breast cancer and ovarian cancer. Moreover, better awareness and detection rates have contributed to the increasing numbers of cancer in women in India.” His colleague Dr Rajesh Dikshit, who heads the epidemiology department, pointed out that if incidences of breast and cervical cancers are removed, women have a very low and almost negligible incidence of cancer in comparison to men.
“Claims from men are usually limited to oral cavity and lungs, where the root causes are tobacco and occupational exposure to hazardous material such as asbestos and silica. We find men who suffer from these cancers come from classes that primarily stay away from taking any health insurance,” said Amit Bhandari of ICICI Lombard.
Interestingly, data for 2014 from Metropolis Healthcare, a chain of laboratories, shows how different cancer rates are among men and women (see box). Dr Kirti Chadha from Metropolis India said of the 1,151 samples that tested positive for cancer in Mumbai, 214 were of breast cancer alone. “Breast cancer is the most common or largest cancer in our country.
This is our finding from each of our laboratories across the country,” she added. There is an age difference pattern too in cancer’s gender bias. “If you look at age-wise cancer incidence, the peak period for women is 60 while for men it is 70,”said Dikshit.
A 2006 paper from Duke University in US titled, ‘Difference between male and female cancer incidence rates: How can it be explained?”, said the peak of hormonal imbalance in women is between 45 and 55, when the reproductive system ultimately stops functioning. In males, this peak is shifted to 55 and 65.
"Global Burden of Cancer"-2013
The Times of India May 29 2015
Sushmi Dey
Deaths in India from the disease have gone up by 60%
Cancer is the 2nd biggest killer
Cancer has emerged as the second-leading cause of death globally after cardiovascular diseases.Proportion of deaths due to cancer around the world increased from 12% in 1990 to 15% in 2013 while the number of new cases almost doubled in India during the period. In India, deaths from the disease have increased by 60%, according to the latest report `Global Burden of Cancer-2013', released worldwide.
“Even if we adjust for the rise in population in India over this period, the new cancer cases have increased by 30% per unit population and deaths have risen by 10%,“ says Lalit Dandona, co-author of the study and Professor at the Public Health Foundation of India and Institute for Health Metrics and Evaluation.
In 2013, there were 14.9 million new cancer cases regis tered globally, whereas 8.2 million people died due to the disease. The report is based on a global study of 28 cancer groups in 188 countries by a consortium of international re searchers from University of Washington and Institute of Health Metrics and Evaluation.
The report suggests that new cases of virtually all types of cancer are rising in countries globally -regardless of income -but the death rates from cancer are falling in many countries primarily due to prevention and treatment. However, it says there is a threat of increasing incidence in developing countries due to ill-equipped health systems.
While incidence of breast cancer is highest in India as well as globally, most number of cancer deaths in India are caused due to stomach cancer, which is globally the second most common reason for death.
Treatment, advisories
Causes of cancer in India, likely preventive measures
See graphic, The principal causes of cancer in India, suggested preventive measures

From The Times of India, September 27, 2017
Ancient Chinese ink, to kill cancer cells
Peter Dockrill, September 28, 2017: Sciencealert
Ancient Chinese Ink holds a surprising new way to kill cancer cells
For centuries, Chinese artists and calligraphers have used their inks to tell countless stories of the world we live in – and now their medium could have a new purpose.
Scientists have discovered that a traditional plant-based Chinese ink called Hu-Kaiwen ink contains distinctive molecular properties that aren't just suited to inscribing messages on paper – they're also ideal for killing cancer cells.
A Chinese team led by researchers from Fudan University in Shanghai began looking into Hu-Kaiwen ink (aka Hu-ink) after noticing its similarities to artificial nanomaterials used in an emerging cancer treatment called photothermal therapy (PTT).
PTT involves injecting substances containing these nanomaterials into tumours in the body, which are then targeted by a laser. Once the laser hits the nanomaterial package deployed in the cancer cells, the cells heat up and die.
Minimising hair loss
Jyoti Shelar, Jan 19, 2017: The Hindu

Tata Memorial begins clinical trials to beat chemotherapy hair loss
The Tata Memorial Hospital (TMH), Parel has started a clinical trial using technology to minimise hair loss due to chemotherapy. The initiative, the first such in India, is expected to address the loss of self-esteem and confidence that many cancer patients, especially women, face and reduce cancer-related trauma.
The trial, which involves four breast cancer patients initially, uses a scalp cooling technique to restrict chemotherapy medication from reaching the scalp, thus reducing hair fall. The machine has two scalp coolers, which are essentially specialised inner silicon caps containing coolants at temperatures of up to minus four degrees centigrade. The technique is widely used in the U.K. and the machine hase been brought to India free of cost.
The machine circulates the coolant in the caps, reducing its temperature and consequently blood supply to the scalp. As chemotherapy medication is given intravenously and circulated through the blood, the scalp gets less blood and thus less of the medication.
The trial is being headed by Dr. Jyoti Bajpai, associate professor, Department of Medical Oncology, TMH. She says chemotherapy medication works best on fast-dividing cells. Since cancer cells divide rapidly, the medicines attack those cells, but other cells like those in the blood, mucosal lining and hair follicles also come under attack.
“This is why patients suffer from reduced blood count, mouth ulcers and hair loss during chemotherapy. But of all the side-effects, hair loss has the worst impact on women. The fear of cancer becomes secondary and the fact that they will lose hair during treatment takes centrestage,” adds Dr. Bajpai.
Doctors grade chemotherapy-induced alopecia, or baldness, in three stages: Grade 0 for no hair fall, Grade 1 for less than 50 per cent hair fall and Grade 2 for more than 50 per cent hair fall (patients need a wig or head scarf). While hair loss starts soon after the first cycle of chemotherapy, there is none in a few cases.
“Through the trial, we are aiming at 50 to 70 per cent hair preservation. In Grade 1, women still feel confident as they are able to mask their scalp with the hair. We want to avoid the Grade 2 stage,” says Dr. Bajpai. The most common side-effects of using scalp coolers are headache and cold, but so far, none of the participants have reported these to be unbearable. The participants feel hair loss is a continuous reminder of the cancer and puts them in focus in a crowd.
Women participating in the trial will begin using the scalp cooler 30 minutes before starting chemotherapy and continue for an hour to 90 minutes after it has been completed. Doctors are maintaining pictorial records to evaluate the scalp cooler’s effect during every cycle. Trial subjects are asked to wash their hair well and not use hair oil on chemotherapy day, and their hair is covered with conditioner before the cap is put on.
The randomised trial, to be conducted over a year, has two arms: one with 34 patients who will be put on scalp coolers, and the other with 17 patients who will not be using the machine. All participants will start the trial from the first chemotherapy cycle. “We are taking non-metastatic patients in whom the cancer hasn’t spread. Also, to maintain uniformity, we have taken patients who are on Taxane- and Anthracycline-based chemotherapy,” Dr. Bajpai says. She adds that usually, patients are administered chemotherapy in two phases: four cycles of Anthracycline-based treatment before surgery and four three-weekly cycles or 12 weekly cycles of Taxane-based medication after surgery.
Dr. Bajpai cites the example of a 35-year-old woman who delayed cancer treatment as she did not want to suffer hair loss. “Another woman from Uttar Pradesh in her fifties was thrown out of her house by her husband and in-laws because of her baldness. Her teenaged daughters were also asked to leave with her. The family considered her disease and baldness to be an outcome of past sins,” she said, adding misconceptions and stigma attached to hair loss are worrying. “Women associate their femininity with hair. It becomes difficult to explain that the hair loss is temporary. Hopefully, such women will be benefited if our trial shows promise.”
Vitamin C: helpful to treat cancer
From the archives of The Times of India: 2008
Vitamin C might be useful to treat cancer after all, according to a US study in which injections of high doses of it greatly reduced the rate of tumor growth in mice. The idea that vitamin C, also known as ascorbic acid, could be used to treat cancer was advanced in the 1970s by American scientist Linus Pauling, who awarded the Nobel Prize in chemistry in 1954. The notion was controversial and subsequent studies failed to show a benefit. But those studies involved vitamin C given orally. The new study involved injections of vitamin C to enable greater concentrations of it to get into the system. The researchers implanted three types of aggressive cancer cells into laboratory mice — ovarian, pancreatic and glioblastoma brain tumors.
Types of cancer affecting India
2012: gallbladder cancer increases
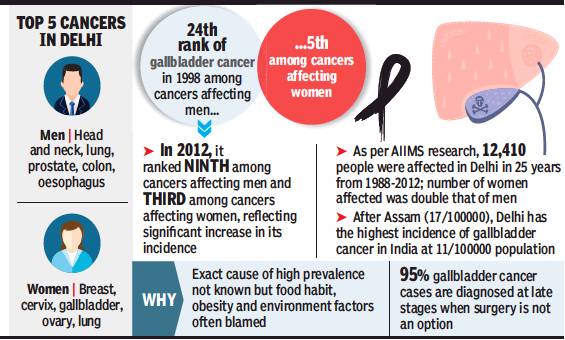
From: DurgeshNandan Jha, In 14 yrs, gallbladder cancer moves up 15 ranks to 9th in men, August 13, 2018: The Times of India
In 1998, gallbladder cancer (GBC) was ranked 24th among all cancers affecting men and fifth among those affecting women in Delhi. In 2012, 14 years later, the ranking of GBC went up to ninth and third for the two genders, respectively.
This alarming finding is part of a report compiled by researchers at AIIMS who analysed 25-year-long data on GBC cases in Delhi under the population-based cancer registry programme of the government.
The exact cause of spike in GBC cases is not known, doctors said, adding that rising obesity and environmental factors may have contributed to this worrying trend. Dr G K Rath, professor and head of AIIMS’ Bhim Rao Ambedkar Institute Rotary Cancer Hospital (BRAIRCH), said Delhi ranks second in GBC prevalence in India with 11cases per 1lakh population. Kamrup district in Assam has the maximum of 17 cases per 1 lakh population.
“GBC remains one of the deadliest cancers. Most cases are diagnosed very late, when surgery cannot be done, and 95% patients die within a year of diagnosis,” Rath said.
The gallbladder is a small, pouch-like organ found underneath the liver. It stores bile, liquid produced by the liver, which helps break down fatty foods. Bile is the main source for removing toxic metabolites.
Data of population-based cancer registries reveal that north India, especially the Ganga belt and eastern India, have high incidence rates compared to other parts of the country.
“No one knows the exact reason why GBC is so common in north India. We are doing a study of genetic analysis of cancer patients from this region. It will be compared with the genes of people from other areas,” Dr Rath said. He added that Indian Council of Medical Research (ICMR) is funding the research to find a solution or a preventive line.
GBC is closely associated with gallstones. But there are other modifiable risk factors that experts said, if reduced, can help lower the disease burden. This includes obesity, smoking, alcohol, dietary pattern and exercise.
A meta-analysis of observational studies found that smokers had an increased risk of developing GBC as compared to non-smokers. “A recent survey also showed that smoking increased by 220% in men from 1998 to 2010, whereas it doubled in women during 2005-10,” said a doctor. He added that fast food, fried food and a sedentary lifestyle is growing among urban Delhi population, especially among the young during the last two decades which may have added to the GBC risk.
In the AIIMS study, published recently in Indian Journal of Cancer, the researchers said that excretion of environmental carcinogens in bile increases the likelihood of GBC.
“The main source of drinking water for Delhi is Ganga and Yamuna. Both these rivers are now contaminated with industrial waste and contain heavy chemicals such as chromium and lead. The Indian government is taking steps to improve water quality of these rivers, but these plans are still on paper and awaiting implementation,” the study said.
2017, an increase
Cancer cases as well as mortality are increasing rapidly among Indian women, primarily because of low awareness and late detection. India accounts for the third highest number of cancer cases among women after China and the US, gro wing annually at 4.5-5%, new data shows.
According to a report `Call for Action: Expanding cancer care for women in India, 2017', cancer among women in India is estimated at 0.7 million. However, the real incidence is much more -between 1 and 1.4 million per year as many cases go undi agnosed or unreported.
India also ranks among the top two countries globally on mortality for key women-specific cancers. Data shows cervical and breast cancer mortality rates in India are 1.6 to 1.7 times higher than maternal mortality. It highlightes the significantly adverse mortality rates for women-specific cancers in the country . India topped the list for mortality for breast and cervical cancers and reported the second highest incidence for ovarian cancer globally .
According to the report, released by E&Y in association with Ficci Flo, in 2015, cancers of the breast (19%), cervix uteri (14%) and ovary (7%) contributed to 40% of all cancer incidence among women with states such as Kerala, Tamil Nadu and Delhi having the highest incidence for these cancers.
“It is alarming that awareness levels of womenrelated cancers is low among the general population and even medical professionals. Despite the established benefits of screening, coverage in India is low for women,“ the report said. India-based studies have confirmed that screening improves early detection of cancers by 1.5-2.5 times. For instance, cancers such as breast and cervical can be cured if detected early and treated adequately .
According to the report, of the 2,000 new women diagnosed with cancer every day , 1,200 are detected in late stages. This reduces fiveyear survival rate by 3 to 17 times for breast and cervical cancer. Late detection also adds to the cost of treatment.Estimates show treatment cost for late-stage cancers is 1.5 to 2 times higher than the cost for early-stage cancers.
In fact, the mortality to incidence ratio, which is a key indicator for measuring effectiveness of national cancer control programmes, is the worst in India for key womenspecific cancers when compared to global peers. Experts say it is imperative to address the menace of growing incidence of cancer among women with urgency and in a holistic manner with due emphasis on prevention, timely diagnosis, effective treatment and palliative care.
The report estimates the economic burden of cancer care treatment to be the high est compared to all other dis eases, with the cost of a sin gle hospitalisation exceed ing the average annual per capita expenditure of more than 60% of the population.
It also projects cancer incidence among women in India to increase from 110 per 1 lakh population to 190-260 per 1lakh population by 2025, which will mirror incidence rates of China and other upper middle income countries such as Brazil and Thailand.
India witnessing further deterioration of key risk factors that contribute to cancer incidence. For instance, while obesity is considered a major contributing factor for cancer, the proportion of overweight women in India grew at twice the global average growth between 2004 and 2014, the report says.
