Doctors in India
This is a collection of articles archived for the excellence of their content. |
Assaults on doctors, patients
Sexual attacks on patients
As in 2024
Rema Nagarajan, August 27, 2024: The Times of India
■ Feb2024— A 24-year-old undergoing treatment for lung infection in the ICU of a hospital in Alwar was sedated and raped by a male nurse.
■ July 2024—A 50-year-old foreign national who had recently undergone surgery was sexually assaulted in a prominent hospital in Gurgaon by a nursing attendant.
■ July 2024— A 25-year-old woman was raped by a doctor while she was unconscious in the operation theatre in a hospital in Pratapgarh.
■ July 2024— A woman recovering from surgery was sexually assaulted by a male physiotherapist in a hospital in Kozhikode.
■ Aug 2024— Two women were sexually assaulted by a cardiology resident doctor in SCB Medical College Cuttack.
Sexual assault of patients inside hospitals is far from uncommon as is clear from these newspaper reports of cases from across India. Yet, there have been no studies on sexual assault of patients. On the other hand, there is an abundance of studies and research on violence that health workers, especially doctors and nurses, suffer at the hands of patients and/or their relatives.
In fact, there is hardly any research on violence of any kind against patients in India, whether verbal, physical or sexual, with the exception of a few studies on ‘obstetric violence’ defined as violence against women by health care providers during childbirth, and on violence against patients with psychiatric ailments. In the few studies that exist, even sexual assault or molestation of patients is described euphemistically as “sexual boundary violations”. Similarly, there is some pushback against the use of the term obstetric violence with a preference for the term ‘mistreatment’.
In the context of obstetric violence, studies have record- ed how patients and their relatives are verbally abused and humiliated by healthcare providers and how they are physically abused in the way pelvic examinations are done and the general ‘rough treatment’ meted out to the pregnant women. However, patients’ advocates point out that such verbal and physical abuse is common even in non-obstetric settings in the hospital.
TOI sought the help of several health researchers to look for studies on violence against patients. “The literature is scarce. Why would perpetrators document their wrongs?” asked one of the researchers. Most of the research on healthcare is done by health providers and they are unlikely to be researching their own wrongdoings, remarked another.
“Medicine in India is paternalistic and the providers don’t feel the need to involve patients as equals in the process of treatment. There are so many forms of violence against patients, both system- ic and structural, and they need to be documented, just like in the studies on violence against health workers, and the reasons and the context need to be studied. The violence is an open secret that is all too familiar to patients, but somehow there is no appetite for research on this.
Patients are powerless and their families are mostly scared to speak up as they fear retaliation against their loved ones who are in the care of the hospital and at the mercy of the doctors and nurses. There is no system for grievance redressal and hence no data on the violence they face,” said Malini Aisola, of the Campaign for Dignified and Affordable Healthcare.
“Independently validated and objective reporting of patients’ concerns does not exist; in the given climate, no organisation is prepared to report the data publicly, even if it collects data properly in the first instance,” observed a rare study on patient safety in India.
AYUSH systems
Allopathy and AYUSH doctors must have the same pay: SC
Dhananjay Mahapatra, August 4, 2021: The Times of India
The Supreme Court ruled that no government can discriminate between practitioners of allopathy and Ayurveda, Yoga & Naturopathy, Unani, Siddha and Homoeopathy (AYUSH) and directed the North Delhi Municipal Corporation to pay AYUSH practitioners on par with allopathy doctors under the Central Health Scheme.
A bench of Justices L N Rao and Hrishikesh Roy said if the central government has enhanced the retirement age of allopathic practitioners to 65 years and it has been implemented by NDMC, it cannot deny the AYUSH practitioners employed under it the benefit of increase in the age of superannuation.
NDMC contended that classification of AYUSH doctors and doctors under CHS under different categories was reasonable and permissible in law. Rejecting the argument, the bench said, :This however does not appeal to us and we are inclined to agree with the findings of the Tribunal and the Delhi High Court that the classification is discriminatory and unreasonable since doctors under both segments are performing the same function of treating and healing their patients.”
Writing the judgment for the bench, Justice Roy said, “The only difference is that AYUSH doctors are using indigenous systems of medicine like Ayurveda, Unani, etc and CHS doctors are using allopathy for tending to their patients. In our understanding, the mode of treatment by itself under the prevalent scheme of things, does not qualify as an intelligible differentia. Therefore, such unreasonable classification and discrimination based on it would surely be inconsistent with Article 14 of the Constitution.”
Availability of Doctors
2010-11: India world’s top supplier of doctors
Sources:
1. The Times of India, Sep 24 2015
2. The Times of India, Sep 24 2015, Lubna Kably
India top supplier of docs to west
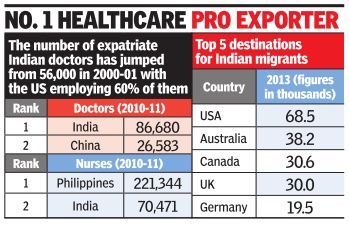
India remains the top sup plier of expatriate doctors to 34 Organisation for Economic Co-operation and Development (OECD) countries, followed by China, reports Lubna Kably. According to a recent report, 86,680 Indian expatriate doctors worked in OECD countries, which include the US and EU bloc, during 2010-11 -up from 56,000 in 2000-01. The US employs 60% of expat Indian doctors; the UK is the second leading employer.
Philippines provided the most number of nurses at 2.21 lakh followed by India (70,471).
2014-15: states with the most, least doctors/ medical colleges
Rema Nagarajan, October 6, 2018: The Times of India
From: Rema Nagarajan, October 6, 2018: The Times of India
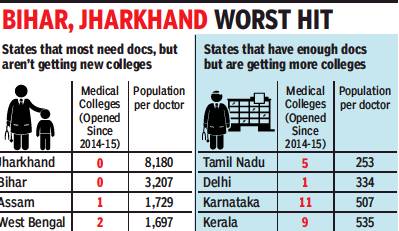
States like Jharkhand and Bihar with acute shortages of doctors have seen few new medical colleges being open in the last five years, while those with a glut of MBBS seats and doctors continue to allow new private colleges. This is despite doctors’ associations warning against overproduction of doctors.
In Jharkhand, a state with the worst doctor-population ratio of just one doctor for over 8,000 people, no medical college has been started since 1969. Even in the last five years, which saw over 121 colleges being opened nationally, Jharkhand got none.
In contrast, Kerala, already facing a glut of doctors with a doctor for 535 people, had nine colleges opening in the last five years, including 6 private ones accounting for 750 seats.
But what can states do about where the private sector chooses to open medical colleges? For any medical college to be opened, the state has to issue an “essentiality certificate”, which certifies that a college is needed. The idea is to prevent unhealthy competition. This raises the question of why states producing more than enough doctors continue to hand out essentiality certificates.
The results are showing in Karnataka where many colleges are in the news for getting fake patients during inspections since they don’t have enough to meet the norms. Many colleges that are allowed to admit students in the first year or for a few years are then derecognised when they no longer meet the MCI norms.
In Karnataka and Kerala, doctors’ associations have warned the governments against starting medical colleges as the glut of doctors is leaving many unemployed.
New private colleges opening creates another problem. The essentiality certificate guarantees if the new college is disallowed admissions by the MCI in a subsequent year, the state government will take over responsibility for students already admitted. This has two effects. First, students who did not get into the much sought after government colleges get entry through the back door. Second, the teacher-student ratio takes a hit at these colleges.
Density of doctors: 2017

From: Rema Nagarajan, 6 states have more docs than WHO’s 1 doc/1k people norm, September 2, 2018: The Times of India
Yet Rural Areas Remain Underserved
Even as governments cite shortage of doctors to allow more private medical colleges, six states — Delhi, Karnataka, Kerala, Tamil Nadu, Punjab and Goa — have more doctors than the WHO norm of one for 1,000 people. Yet, some can’t find enough doctors for rural public health system. Also, most doctors from these states are unwilling to move to states like Bihar or UP that suffer from an acute shortage. This again raises the question of whether merely producing more doctors can address the crunch in public health and in rural areas.
The density of doctors per 1,000 people in Tamil Nadu is as high as 4, almost at the same level as countries like Norway and Sweden, where it is 4.3 and 4.2 respectively. In Delhi, the density is 3, higher than the UK, US, Canada and Japan, where it ranges from 2.3 to 2.8. In Kerala and Karnataka, the density is about 1.5 and it is about 1.3 in Punjab and Goa.
TOI calculated these densities after deducting 20% from the number of registered doctors, as is done by the Medical Council of India to estimate the number of doctors available, since many state councils have not updated their registries. In states that have updated them through periodic reregistration, as in Delhi, the 20% reduction was not applied.
Since India’s doctors are largely concentrated in urban areas, it is possible that even some states with doctor population ratios better than 1:1,000 may have shortages in rural areas. However, Tamil Nadu and Kerala boast that they have no vacancies in their rural public health systems.
According to Dr Prabhakar DN, former president of the Karnataka branch of the Indian Medical Association, 40% of doctors in Karnataka are in Bangalore. “In rural areas, there is still a shortage. Bangalore is saturated, even for specialists. So they don’t get jobs. Doctor salaries are coming down... We need to focus on producing doctors for the periphery. Just producing more doctors won’t work,” he added.
“Unlike engineers, who typically need to find jobs, doctors can be self-employed. If there are too many in a geographical area, they resort to unethical practices on the few patients they get to make ends meet. That’s why there is a need to calibrate the number being produced. We have told the state government to stop allowing the opening of more private colleges. They should shut down many of those that are in a bad shape, with no patients and no money to pay their faculty. The IMA is having to intervene each time to help them as they are not paid for six to eight months,” said Dr N Sulphi, secretary of the Kerala IMA.
2018/ 82% shortfall in specialists
Sushmi Dey, July 1, 2019: The Times of India

From: Sushmi Dey, July 1, 2019: The Times of India
The crisis in India’s public health infrastructure is laid bare by stark official statistics that reveal that the country faces a shortfall of around 82% in specialists like surgeons, gynaecologists, physicians and paediatricians, almost 40% in laboratory technicians and a critical 12-16% shortage of nurses and pharmacists at community and public health centres (CHCs and PHCs).
In most states, the gap between required and available specialists in these centres, which are often the first port of call and are also expected to act as early warning and referral systems, is in the range of 80-99%. For instance, Himachal Pradesh, Haryana, Uttar Pradesh, Chhattisgarh, Gujarat, West Bengal and Kerala have a 90% plus shortfall. Other large states like Bihar, Jharkhand and Tamil Nadu have over 86% shortage of such doctors. The statistics provide compelling evidence of increasing dependence on private healthcare which is costlier, and point to the need for larger involvement of the private sector as partners in gover nment programmes as also the urgent task of improving service conditions and incentives in PHCs and CHCs. With the deaths of more than 150 children due to AES in Muzaffarpur a grim reminder, the data shows a national picture that requires strong policy responses.
While the overall data shows that there is not much of a gap in demand and supply of nurses and pharmacists, a closer look reveals huge disparity among states. So, while there is 12.6% shortage of nurses with almost all UTs and smaller states having a surplus, states like Himachal Pradesh, Bihar, Uttarakhand, Maharashtra, Odisha and a few others have a shortages ranging from an average 45% to 63%, data provided to Parliament shows.
Government data points out a serious shortfall of laboratory technicians – who play a crucial role in diagnosis and early detection of diseases – in public health facilities. States like Himachal Pradesh, Uttarakhand, Chhattisgarh and Uttar Pradesh have major deficits, while only some smaller states like Meghalaya, Mizoram and UTs have adequate numbers. In total, there are 19,434 laboratory technicians or 62% of the total 31,367 required at PHCs and CHCs.
“Primary care is incomplete without efficient response capacity of CHCs to timely address referral needs,” said R K Srivastava, former Director General Health Services.
2019: the position in the states
Pushpa Narayan, August 7, 2019: The Times of India

From: Pushpa Narayan, August 7, 2019: The Times of India

From: Pushpa Narayan, August 7, 2019: The Times of India
India should in six years meet the WHO benchmark of one doctor per 1,000 people, but the national average hides deep imbalances where individual states are concerned Long queues outside doctors’ clinics, overcrowded hospitals and the huge backlog of patients for surgeries clearly suggest that the country needs more doctors. The data shows that India needs 4.3 lakh doctors added to its existing pool to reach the WHO standard of doctor–patient ratio of 1:1,000 instead of the current 1:1,499.
With an annual output of nearly 80,000 doctors, the country should meet the WHO norm within the next six years. But like most things in our healthcare system, this is complicated too as the shortage isn’t uniform across all geographical terrains. Maharashtra, Kerala, Andhra Pradesh, Karnataka, Tamil Nadu and Punjab already have more than one doctor per 1,000 people.
But the situation in Bihar, Chhattisgarh, Jharkhand, UP and Madhya Pradesh is deplorable. At the current rate at which their colleges are producing doctors, Bihar will take at least 56 years to achieve WHO standards and Jharkhand more than 87 years.
Even in states with the required number of doctors, there are districts with poor health indices because doctors crowd the cities. For instance, Tamil Nadu has declared 16 of its 32 districts backward on various health indices, primarily due to doctor shortage in the rural areas.
Thus, India needs more medical schools, but at the right places, and to produce doctors willing to serve where they are most needed. States with poor doctor-patient ratio, for instance, should have innovative policies and attractive salaries for doctors from other states to move in. It may not be immediately possible for a state to add more medical colleges without having experienced doctors to fill faculty positions. Such states may have to tie up with others to carve out a quota for their students with a condition that these students will return to serve in their home state.
MCI list, 2018: outdated but has historical nuggets
MCI Record Not Up To Date, Lists Even Those Who Registered In 1915
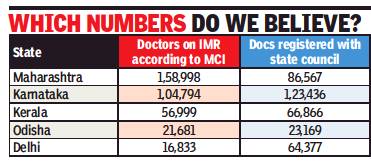
How many doctors does India have? Going by data given to Parliament by the Medical Council of India (MCI), there are more than 10.8 lakh doctors registered. In reality, no one really knows as is evident from the MCI’s own answer that 80% availability has to be assumed from this total number.
Why 80% and not 90% or 75%? A look at the Indian Medical Registry (IMR) makes it clear why no one knows exactly how many doctors are alive and practicing. Here are a few examples of doctors found in the registry.
Dinabandhu Basak, who qualified as an LMF (licenciate of medical faculty) from the University of London in 1895, and registered with the West Bengal Medical Council in 1915; Surendra Chandra Majumder, LMP (licenciate in medical practice) from Dibrugarh University in 1907, who registered with the Assam Medical Council in 1920; Shashi Bhushan Dutta, LMS (licenciate in medicine and surgery from Calcutta University in 1911, registered in 1918 with the Bihar Medical Council; Captain Christian Salvadore, MBBS from Kerala University in 1914, registered with the Travancore council in 1945; Y Sheshachalam, LMP from Madras University in 1916, registered in 1955 with the Andhra Pradesh council.
Over 75,000 of the doctors in the IMR registered before independence or a little after it, some as early as the 19th century as the examples given show. It seems safe to assume that a majority of them are dead or not practicing any more. Yet their names remain on the register and are counted year after year. Repeated directions since at least 2009 to state councils to re-register all doctors to weed out those who might have died, migrated, or stopped practicing have yielded little or no result.
One council with a live register is the Delhi Medical Council. But in this case, the data given to Parliament shows just 16,833 doctors registered in Delhi while the DMC itself says there are over 64,000. DMC president Dr Arun Gupta explained: “We have 48,657 re-registrations and 15,720 first-time registrations. Thus a total of 64,377 doctors registered with our council. So we have a fairly good idea of the actual number of doctors in Delhi.”
Unlike Delhi, MCI says many states like Haryana, Bihar, Orissa and Karnataka have not sent it the registration data for several years. “The State Medical Councils are established under an Act of the respective state legislatures. They are independent statutory authorities and MCI does not enjoy any supervisory role or control over them,” explained MCI President Dr Jayshree Mehta. According to the Indian Medical Council Act of 1956, under which the MCI is constituted, it is the statutory duty of the council to maintain the IMR. The Act also mandates state councils to supply MCI with a copy of their registers after April 1 of each year with all additions and amendments.
As a result, year after year, Parliament is given the same meaningless data without any effort by the health ministry, MCI or state councils to clean it up. Why does this matter? The health ministry calculates the shortage of doctors based on this data. In the age of Digital India and Aadhaar, it seems inexplicable that the government is unable to maintain a database of barely 10 lakh doctors.
Last year, the MCI had tried to initiate a system of Unique Permanent Registration Number (UPRN) for every doctor to be able to track them in cases of medical negligence, to get a clearer picture of how many doctors are practicing in India and to tackle the menace of fake doctors or ones with unrecognised degrees. The fact remains that over 60 years after it came into existence, the MCI has been unable to do the basic function of getting the IMR right.
Actual numbers: MCI vs. state councils
From: Rema Nagarajan, State councils blame MCI for mess in data on doctors, August 16, 2018: The Times of India
Several State Medical Councils have expressed shock at the Medical Council of India (MCI) submitting outdated and wrong data to Parliament year after year.
According to the officebearers of these councils, they have been sending updated lists to the MCI but do not see it reflected in the Indian Medical Register (IMR). Maintaining the IMR is one of the fundamental and statutory duties of the MCI.
While the MCI told TOI the state councils were to blame for not regularly sending information on registered doctors to it, most state councils refuted this allegation.
In the case of Karnataka, for instance, the MCI data submitted to Parliament recently showed 1.04 lakh doctors registered. The data MCI gave TOI also said the state council had not submitted any data in 2015 or 2016. However, the state council insisted it has been submitting data every quarter. The Karnataka Medical Council started the process of re-registration of doctors every five years in 2013 and after renewal had about 123,436 doctors in the registry as of March 2018, nearly 20,000 more than the MCI data shows.
“It is disrespect to Parliament to not make any effort whatsoever to give the latest data and not even explain to Parliament that the data being submitted has not been updated,” said KMC president, Dr H Veerbhadrappa.
The Maharashtra Medical Council (MMC) has not only done the process of reregistration of doctors every five years, the entire list of 86,567 doctors registered with it is available on the council’s website. “We have the most modern system. The revalidated data has been shared with the MCI, but it is still not reflected in the IMR,” said MMC president Dr Shivkumar S Utture. The MCI data shows 1.59 lakh doctors in Maharashtra, nearly twice as many as the state council’s number.
The MCI responded to the state councils’ claims by insisting the Karnataka figures it had put out were correct and that in Maharashtra’s case the state council had submitted no data for 2016 and data in a “wrong format” for 2017 only this month. It said, “as per the office records, we assure you that no wrong information has been submitted to the parliament.”
Since Karnataka and Maharashtra have a large number of medical colleges, they have many out-of-state students registering with these councils immediately after completing MBBS. But then they take no objection certificates (NOC) and go to their respective states. The NOCs issued are tracked and the names are removed from the register.
“Even office-bearers of the Travancore-Cochin Medical Council that registers all doctors in Kerala, who have sent their details to the MCI so many times find their names have not yet been included in the IMR. Then you can imagine just how well they are maintaining the database,” pointed out Dr VG Pradeep Kumar, vice-president of the council.
STATE-WISE
2019: The states with the most doctors
July 13, 2019: The Times of India
One in eight doctors across India is from Tamil Nadu
CHENNAI: Nearly one in eight doctors in the country is from Tamil Nadu. The state, which has 12% of the total number of doctors in the country, is second only to Maharashtra, which has about 15% of the total number of doctors, according to Union health minister Harsh Vardhan in Parliament. Almost simultaneously, the issue was debated in the assembly on Friday.
Responding to questions raised by Congress MP Mohammed Javed on the shortage of doctors in the country, Harsh Vardhan told Parliament that as per Medical Council of India (MCI), there were 11.59 lakh allopathic doctors registered with the state and MCI until March 31. “Assuming 80% availability, it is estimated that around 9.27 lakh doctors may be actually available for active service,” he said. This would mean a doctor-population ratio of 1:1456 as per the population estimate of 1.35 billion, lower than the WHO norm of 1:1000, he added. On its part, the Union ministry enhanced the maximum intake capacity at MBBS to 250 seats, relaxed norms for setting up medical colleges in terms of requirement of land, faculty, staff, bed strength and other infrastructure and strengthened existing state government colleges to increase medical seats, the Union minister said.
Tamil Nadu has 1.3 lakh doctors, compared to 1.7 lakh doctors in Maharashtra. There are 1.2 lakh doctors in Karnataka and about a lakh in Andhra Pradesh. With 77,549 doctors Uttar Pradesh was among the top 5 states with maximum number of doctors.
“If you compare the number of doctors with the population, Tamil Nadu is far better than any other state,” said TN Medical Services Corporation MD Dr P Umanath, who headed a committee that prepared a report on how to incentivise doctors working in rural and remote areas of the state. Tamil Nadu has 23 government medical colleges that offer 3,250 MBBS seats. Beside, there were at least 2,050 seats in government-run private colleges and self-financing colleges and an almost equal number of seats in deemed universities.
However, just like the rest of the country, the distribution of doctors is not uniform in TN, he admitted . This was the concern raised by MLAs in the assembly on Friday. They said many primary health centres in their constituencies either have no doctors or don’t have adequate number of doctors.
DMK MLA from Mailam R Masilamani, a doctor himself, said, “We want the health department to appoint sufficient doctors for PHCs in our areas. They must be open for patients round the clock.” Congress legislative chief K R Ramaswamy said several posts in the Sivaganga Medical College Hospital and other government hospitals were vacant. Health minister C Vijayabaskar said government doctors were appointed through a medical recruitment board and through TNPSC. “It is a continuous process. Soon, vacancies in all hospitals will be filled,” said the minister. Tamil Nadu, officials said, was aware of the dearth of doctors in rural areas. “While there are more number of doctors in cities and tier-1 cities, the number of doctors in rural and remote areas is very low. This is why Tamil Nadu tries to incentivise doctors working in difficult terrain. Government doctors working in these areas get additional marks during PG admissions,” Umanath said.
Delhi, 2019: a shortage in govt. hospitals

From: Abhinav Garg, Durgesh Nandan Jha, Lack of doctors puts Delhi's hospitals on life support, April 5, 2019: The Times of India
A status report filed by the state government in Delhi high court says there is an acute crisis of manpower in Delhi’s state-run hospitals. For instance, in GB Pant Hospital, the largest of the government’s super-specialty institutions, 159 posts for doctors are vacant, while the paramedical/nursing and non-medical strengths are short by199 and 233, respectively.
The situation in LNJP, Deen Dayal Upadhyay, Ambedkar and Guru Tegh Bahadur hospitals, among the biggest tertiary care centres in Delhi, are not reassuring either. The status report says that in LNJP, there are 41 vacancies among doctors, 15 among paramedical staff and 229 among the non-medical staff. Hospital sources said the figure for doctors related only to non-teaching specialists.
The report was filed in response to the persistent queries of the bench of chief justice Rajendra Menon and justice V K Rao, which had sought to know last year about the specific steps taken by the government to improve health facilities. The bench is hearing a PIL filed by Madhu Bala, a schoolteacher in Karawal Nagar who lost her baby after admission to GTB Hospital for delivery.
Bala’s lawyer Prashant Manchanda alleged in the petition that the hospital’s woeful infrastructure and lack of medical facilities were behind the loss of the baby and the near death of his client. He claimed the hospital did not perform a crucial surgery pleading “non-availability” of an OT. The petition urged the high court to step in “to immediately resurrect the dangerously dilapidated health system in public hospitals and utilise huge funds to infuse instant course correction and overhauling to prevent further health hazards”.
To begin with, the concerned court demanded details of the “infrastructural facilities available, the requirement of manpower for running of the hospitals and various other issues like functioning of equipment, installation of necessary equipment for treating the patients, etc” at the five hospitals. It directed the government to furnish information on life-saving equipment, drugs, beds, operation theatres and staff, among others. However, at the previous hearing, the court asked for more details as it was not satisfied by the data furnished by Delhi government’s Director General of Health Services on behalf of the hospitals.
“The real crisis is the depleted nursing staff and technicians. There have been occasions when surgeries had to be postponed due to the unavailability of nursing orderlies and safai karamcharis,” admitted a doctor at LNJP, who did not want to be quoted.
According to information furnished by the hospital, there are 436 sanctioned posts for safai karamcharis, of which 167 are currently vacant. There are no x-ray attendants, and the number of operation theatre attendants is also half the sanctioned strength.
In DDU Hospital, the largest government hospital in west Delhi and visited by over 4,000 patients daily, the data compiled by the government and shared with the high court shows a quarter of the posts of regular doctors in the 640-bedded hospital is vacant. The vacancy among the resident doctors and nursing staff is 15% and 10%, respectively.
Kerala has 3.3 times as many doctors as WHO norm/ 2019
From: Preetu Nair, In Kerala’s ‘sick’ hospitals, doctors are first casualty, March 21, 2019: The Times of India
State Has A Doc-Population Ratio Of 1:300 While WHO Prescribes 1:1000
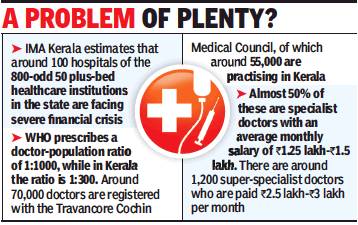
Wedged between corporate hospitals with deep pockets and a vastly improved public healthcare system, mid-level private hospitals across Kerala are either not paying their doctors on time or forcing them to accept drastic pay cuts. In some hospitals, they are even retrenching doctors. The most affected are 50 to 100-bed hospitals. Of the 23 private medical colleges, about five are at present paying their doctors on time.
“It’s true that many hospitals are unable to pay doctors on time. Even senior specialist doctors are affected”, Indian Medical Association (IMA) state secretary Dr N Sulphi said. According to IMA Kerala estimates, of the 800-odd 50 plus-bedded healthcare institutions, around 100 hospitals are facing financial crisis and unable to pay doctors’ salaries.
Ironically, Kerala’s remarkably high doctor-topopulation ratio — WHO prescribes a doctor-population ratio of 1:1000, while in Kerala the ratio is 1:300 — could be at the root of the problem. There are around 70,000 doctors registered with Travancore Cochin Medical Council , of around 55,000 are practicing in Kerala. Of the 55,000, almost 50% are specialist doctors and get an average Rs 1.25 lakh to Rs 1.5 lakh salary per month. The around 1,200 super-specialist doctors in the state get anything between Rs 2.5 lakh and Rs 3 lakh per month. In a good hospital that has been in existence for more than 4 to 5 years, the doctor’s salary constitutes 20% of the total cost.
“Some are even forced to take a salary cut while taking a new job,” Dr Sulphi said. With almost 60% to 70% of doctors working as consultants, they don’t even have proper leave facility. There are no social security measures in place. With more doctors losing jobs, IMA has intervened and asked hospitals to at least honour contracts.
“We spend crores to set up speciality units but often doctors are unable to live up to the expectation and we don’t even get enough money to repay loans. Then we either have to reduce doctor’s salary or close down the unit,” said Kerala Private Hospitals Association (KPHA president Dr PK Mohamed Rasheed.
Kerala state planning board member Dr B Eqbal said, “With facilities in the government hospitals improving, people are opting for government hospitals. From just 25% patients availing services at government hospitals in the past, now it is jumped to 40%”.
Court judgements
2018: HC fines doctors ₹5,000 for poor handwriting
Ravi Singh Sisodiya, October 4, 2018: The Times of India
‘ILLEGIBLE WRITING OBSTRUCTION TO COURT WORK’
Poor handwriting of doctors are not really surprising, but a court in Uttar Pradesh has put that on record now.
A Lucknow bench of Allahabad high court has imposed Rs 5,000 penalty each on three doctors in separate cases for their illegible handwriting.
In the three criminal cases that came up for hearing last week, the injury report of the victims issued by hospitals from Sitapur, Unnao and Gonda district hospitals were “not readable” because the handwriting of the doctors who had issued them were “very poor”.
The bench considered it an obstruction in the court work and summoned the three doctors — Dr TP Jaiswal of Unnao, Dr PK Goel of Sitapur and Dr Ashish Saxena of Gonda. A bench of Justice Ajai Lamba and Justice Sanjay Harkauli admonished them and asked them to deposit Rs 5,000 penalty in the court’s library.
The doctors pleaded they erred in writing legible prescriptions as they were overburdened.
The court further directed principal secretary (home), principal secretary (medical & health) and director general (medical & health) to ensure that in future, medico reports are prepared in “easy language and legible handwriting”. The court also suggested that such reports should be computer-typed.
“The medico-legal report, if given clearly, can either endorse the incident as given by the eyewitnesses or can disprove the incident to a great extent. This is possible only if a detailed and clear medico-legal report is furnished by the doctors, with complete responsibility,” the bench observed.
It added, “The medical reports, however, are written in such shabby handwriting that they are not readable and decipherable by advocates or judges. It is to be considered that the medico-legal reports and post-mortem reports are prepared to assist the persons involved in dispensation of criminal justice. If such a report is readable by medical practitioners only, it shall not serve the purpose for which it is made.”
The court reminded the doctors of a circular issued by UP director general (medical & health) in November 2012 which stipulated doctors to prepare medico-legal reports in readable for m.
Doctor-patient privilege/ physician-patient privilege
Directions to doctor to produce records an infringement of rights
Vasantha Kumar, January 3, 2022: The Times of India
BENGALURU: An illicit relationship of a spouse cannot be proved by securing his or her private medical records, the Dharwad bench of the Karnataka HC has observed in a recent judgement.
“If this approach is to be accepted, (then) it would amount to destruction of the entire concept of doctor-patient confidentiality and drag the doctor into a marital dispute,” Justice NS Sanjay Gowda has said in the order, quashing the March 30, 2021 ruling of a family court in Dharwad.
The order was passed on an application submitted by the husband, seeking summoning of a doctor to produce documents relating to his wife’s alleged abortion. The wife challenged the order, contending that the medical records of a person are “absolutely private” to the person and the same cannot be sought by any person, including the husband. The husband argued he had made an allegation about the “adulterous life” his wife was leading. After hearing both parties, Justice Sanjay Gowda allowed the petition filed by the wife.
The judge noted that the power to direct a medical practitioner to act in violation of his declaration should be exercised only for strong and compelling reasons and would more or less be exercised only when an element of public interest was involved.
Pointing out that medical records of an individual are private and not for public consumption, the judge added that a direction to the medical practitioner to produce the records or divulge information he is privy to would amount to infringing upon the fundamental right of privacy guaranteed to an individual, which emanates from the ‘right to life’ granted under Article 21 of the Constitution.
The ‘Dr’ prefix
Pharm D degree holders can use ‘Dr’ prefix
Chaitanya Deshpande, May 28, 2019: The Times of India
The Pharmacy Council of India (PCI) has decided that candidates awarded the Doctor of Pharmacy degree (Pharm D) from recognised universities will be authorised to use the ‘Dr’ prefix.
“PCI has taken a decision of prefixing ‘Dr’ before the name of candidate who are awarded Pharm D degree. All the universities and examining authorities approved by the PCI are requested to use this prefix while awarding degree certificates,” reads the letter issued to director of board of examination and evaluation of Sant Gadge Baba Amravati University by registrar-cum-secretary of PCI Archana Mudgal.
Pharm D course was started in India in 2008. In Maharashtra, it was launched in 2012. The first batch of the sixyear course passed in 2018. The second batch is scheduled to get the degree in 2019 convocations. As universities in the state were not issuing degrees with ‘Dr’ prefix till now, members of Doctor of Pharmacy Association of Maharashtra had approached the PCI for a clarification. It is not clear when the PCI originally decided on the Dr prefix.
“We have been pursuing this issue for last two years. When university authorities told us they don’t have written directives from the PCI regarding the ‘Dr’ prefix, we wrote to PCI. On May 24, the PCI issued a letter in this regard,” said Vinayak Bhagwat Ghayal, president of Doctor of Pharmacy Association, Maharashtra.
Maharashtra Registered Pharmacist Association has welcomed this move.
According to Pharm D degree holders, using Dr prefix will be helpful for them in many ways. “The ‘Dr’ prefix will differentiate us from the other pharma degree holders. We will get our due recognition in the job market,” said Aniket Bhosale, a Pharma D student.
Emoluments
As in 2020
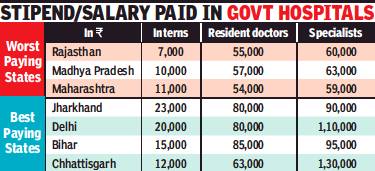
From: Hemali Chhapia, Delhi, UP pay resident docs most, interns in Maha among worst paid, June 8, 2020: The Times of India
Delhi, Uttar Pradesh and Bihar pay resident doctors (MBBS degree holders pursuing postgraduation) the most. Chhattisgarh, Jharkhand, Gujarat and Haryana are also among the better paymasters for doctors at different levels in government-run hospitals. Interns (those in the final year of their MBBS course) in Maharashtra are among the worst paid even after a recent hike; only three other states, Rajasthan, MP and UP, pay lower. And specialists – senior residents pursuing a superspecialty course – are better off in the rural parts of Chhattisgarh, Haryana and UP where they earn Rs 1 lakh to 1.5 lakh a month, compared to Maharashtra where they get an average Rs 59,000.
Interns at Centre-run hosps get highest pay
At a time when resident doctors across the country are on the frontlines attending to Covid-19 patients, there is wide variation in their stipend depending on which part of India they serve. Chhattisgarh pays the maximum. UP, Bihar, Jharkhand, Haryana, all pay Rs 80,000-Rs 1 lakh a month while Maharashtra and the southern states lie in the mid-range, paying a monthly stipend of Rs 40,000-Rs 60,000. The Medical Council of India plans to make stipend post-MBBS uniform across the country, but the plan is yet to be cleared by all states.
Interns posted in central government-run hospitals are paid the highest, Rs 23,500 a month. Across India in staterun hospitals, their stipend varies from as low as Rs 7,000 in Rajasthan to the highest in Karnataka now at Rs 30,000. Medical interns are students who have completed four-anda-half years at a med school and do their compulsory rotational residential internship at a hospital attached to the medical college before getting the MBBS degree.
While interns in Maharashtra get a stipend of Rs 6,000, it was recently hiked to Rs 11,000 by the state. But BMC hospitals in Mumbai are yet to effect the change. Residents and senior residents in the state get Rs 54,000 and Rs 59,000, respectively (average of three years). The BMC recently announced a temporary stipend of Rs 50,000 for MBBS interns for their work in the Covid-19 wards. But a permanent increase of Rs 10,000 is expected for residents, said the head of the Directorate of Medical Education and Research in Maharashtra Dr T P Lahane.
At the postgraduate level, the stipend varies for every state as also for each year of the resident. In some states, there are multiple scales; to attract talent, the stipend offered to residents in rural areas is higher compared to what is paid in urban centres. For instance, in Chhattisgarh, residents in rural areas are paid Rs 20,000-30,000 more and seniors are paid Rs 1.5 lakh as compared to their counterparts in city hospitals who take home Rs 1.3 lakh a month. One of the reasons Bihar, UP, Chhattisgarh and Jharkhand pay government doctors much higher, experts say, is because of the dependence on the public healthcare network in these states as compared to Maharashtra, TN or Karnataka, which have more hospitals driven by charitable trusts and private practitioners.
Founder member of Alliance of Doctors for Ethical Healthcare Dr Babu KV has for long been writing to the MCI for a uniform stipend for interns, residents and seniors.
Health issues
Kerala doctors die earlier than general public
Nov 20, 2017: The Times of India
HIGHLIGHTS
Doctors in Kerala are dying younger when compared to the general public according to a study conducted by Indian Medical Association.
Majority of doctors in Kerala die due to cardio-vascular diseases and cancer.
Life expectancy of an Indian is 67.9 years and that of a Malayali is 74.9 years, the mean ‘age of death’ for a Malayali doctor is 61.75 years
Doctors heal and help people live longer, but it seems many of them are dying younger when compared to the general public in Kerala. A study conducted by research cell of the Indian Medical Association (IMA) in Kerala found that a majority of them die due to cardio-vascular diseases and cancer.
While the life expectancy of an Indian is 67.9 years and that of a Malayali is 74.9 years, the mean 'age of death' for a Malayali doctor is 61.75 years, said the study. "We were surprised by the figures as we expected doctors to live longer as they know what is good for them," said IMA research cell convener Dr Vinayan KP.
For the 10-year study - titled Physician's Mortality Data from 2007 to 2017 - the mortality pattern among doctors enrolled with state IMA's social security scheme was analysed. Of the 10,000 doctors who were part of the contributory supportive scheme that provides a fixed amount to deceased doctor's family, 282 died during the study period.
Of this, 87% were men and 13% women. Almost 27% died due to heart diseases, 25% due to cancer, 2% died due to infection and another 1% committed suicide.
The study didn't look at the reasons for early death, but doctors reasoned that stress was a major contributor. "Doctors are generally working under a lot of stress irrespective of government or private jobs. Increased working hours, the patients they attend to and high expectations contribute to this increased stress. Their working hours need to be fixed, besides government social security scheme. Also doctors should be prepared for periodic health check-ups," said IMA's former president Dr VG Pradeep Kumar.
"Being a doctor in India is injurious to one's health now. Due to stress, doctors are more prone to heart disease, diabetes and even paralysis," said IMA national president Dr KK Aggarwal. While IMA's national study showed that doctors were dying on an average 10 years earlier than the general population; in Kerala - a state with high life expectancy -they die nearly 13 years earlier.
IMA, Kerala is in the process of doing a prospective study on the health profile of all its members - their lifestyle, food habits. It also will see whether doctors themselves go for a regular medical check-up. "The present study is a retrospective study and has its limitations. We don't know the lifestyle and habits of those who died. Also some elderly doctors may not be part of the scheme as it is a voluntary one introduced much after IMA was formed here," said Dr Vinayan.
Health expert Dr B Ekbal (one of the few doctors in the state who is not an IMA member) said that a detailed study covering all doctors was essential before reaching a final conclusion. "This may be an indication about doctor's health, but a detailed study is needed," he said.
Homeopaths
Cannot prescribe allopathic medicines
AmitAnand Choudhary, July 14, 2019: The Times of India
A homeopathic doctor is not qualified to prescribe allopathic medicines and will be liable for medical negligence and will have to pay compensation if a patient suffers from medical complications, the National Consumer Disputes Redressal Commission has ruled.
Almost two decades after a woman died soon after a homeopathy doctor in Nagpur gave injections to her, the apex consumer commission directed the doctor to pay compensation of Rs 10 lakh to her family members saying he is a diploma holder in homeopathy and is not qualified to practise allopathy.
“It is clear that the opposite party (doctor), being a homeopathic practitioner, is not having any authority to administer allopathic medicines i.e. injections. Thus, without any authority he administered the said injections of allopathic medicines and as her (patient’s) death was caused due to reaction of the said injections, it proves negligence on his part,” the NCDRC said.
Medical associations, professional
Representation of women
Rema Nagarajan ,August 14, 2024: The Times of India
Though women outnumber men in medical college admissions, only nine (19.5%) of 46 professional medical associations in India have been led by women. In the largest association of doctors, Indian Medical Association (IMA), out of 92 individuals who have served as presidents since its inception, only one was a woman.
Just six of the medical associations have a 50% or higher representation of women in their current central leadership committee. This was revealed in a study on representation of women in leadership positions in medical associations.
The study published in PLOS Global Public Health stated that considering predominant role of professional medical associations in shaping medical training and health policies in India and beyond, skewed gender representation was a major concern.
“This lack of diverse representation can lead to an unbalanced agenda that may not adequately address the health and care needs of women or sufficiently take into account gender-specific issues when advocating for or collaborating on particular health policy and programmes,” noted the study. Of 64 individuals currently serving as presidents and secretaries of 32 state subchapters of IMA, only three are women.
Six medical associations that had a 50% or higher representation in their current central leadership committee were Indian Association of Palliative Care (100%), Federation of Obstetric and Gynaecological Societies of India (61.5%), Indian Association of Pathologists and Microbiologists (57%), Indian Association of Dermatologists, Venereologists and Leprologists (55.5%), Indian Association of Medical Microbiology (50%), and Academy of Family Physicians of India (50%).
Five associations — Indian Society of Aerospace Medicine, Academy of Hospital Administration, Indian Orthopaedic Society, Indian Association of Gastrointestinal Endosurgeons, and Urological Society of India — have had no women presidents since their inception.
The study concluded that the results were consistent with global studies indicating that although there are more women entering medical field than ever before, very few reach leadership.
National Medical Register
As of 2025
Rema Nagarajan, August 9, 2025: The Times of India
Almost a year after the National Medical Register was launched as “a comprehensive and dynamic database for all allopathic doctors”, only 996 of the 13.9 lakh allopathic doctors registered with state medical councils have got NMR registration. In response to an RTI query, National Medical Commission (NMC) stated that of the 11,200 applications for registration received, 91% have not been approved as of Aug 8.
Launched with much fanfare by Union health minister on Aug 23, 2024, the NMR portal of NMC for registration of all MBBS doctors eligible to practise in India has failed to take off. NMR was hailed as a move to “strengthen the digital healthcare ecosystem”, after which similar registers were to be launched for paramedics and other healthcare professionals. Yet, with the register for doctors — who constitute the smallest professional group in the health system — not materialising, it remains to be seen whether the registers for an estimated 35 lakh nurses and for paramedics, who would be more than double the number of nurses, will happen any time soon.
In response to a question in Parliament, the health ministry said that 13.9 lakh MBBS doctors are registered with state councils, of which it is assumed that about 80% (over 11 lakh) are available.
NMC had issued the Registration of Medical Practitioners and Licence to Practice Medicine Regulations, 2023, on June 8, 2023. According to the regulation, NMC’s Ethics &Medical Registration Board shall maintain the NMR, which shall contain entries of all doctors in all state registers maintained by state medical councils. The regulations envisage a unique identification number for every doctor, centrally generated by EMRB, which will “grant registration in NMR and eligibility to practice medicine in India”.
All existing medical practitioners enrolled in the Indian Medical Register or the State Medical Register not having registration number as per the regulation were mandated to update their registration in the web portal of EMRB within three months of publication of the regulation.
However, applications have petered out as approvals for 90% of those who applied are still pending. From 6,000 applications in the first three months after launch, applications have dwindled to less than 800 in past four months.
The renewal of registration every five years is supposed to happen through state councils and the status of registration in the state registry “shall automatically reflected (sic) in the National Register”. However, state registries are yet to be linked to NMR.
“Even when state councils confirm the membership of a doctor, NMC is rejecting it, as in my case,” said Dr KV Babu, an ophthalmologist and RTI activist. “Why not accept those verified by state councils and make it simple?”
Quacks
57% ‘doctors’ are quacks: Govt, WHO/ 2016
Rema Nagarajan, August 9, 2019: The Times of India
Are 57% ‘docs’ quacks? Govt says no, then yes
Is a majority of those practising allopathy in India quacks? The government said no. But now it says yes. A 2016 WHO report on the health workforce in India had shocked everybody by stating that 57.3% of those practising allopathic medicine did not have any medical qualification. Then Union health minister JP Nadda had rubbished the report as “erroneous” in January 2018 while responding to a query in Lok Sabha. But the data has now gained official approval, with the health ministry using it to argue the case for allowing community health practitioners in the National Medical Commission Act just notified.
The FAQ on the Bill (as it then was) issued by PIB on August 6 said 57.3% of personnel practising allopathic medicine do not have any medical qualification. According to the WHO report based on the 2001 Census, barely 20% of those who practised medicine in rural India had any medical qualification.
31% of ‘allopathic doctors’ educated only up to Class 12
It also estimated that 31% of those who claimed to be allopathic practitioners were educated only up to Class 12.
“The report is erroneous since MBBS is the minimum qualification for enrolment as registered medical practitioner in a state medical register to practise medicine, and hence all registered doctors have medical qualifications,” stated Nadda in a written reply to a Lok Sabha question on January 5, 2018. He was, however, quick to add that “the primary responsibility to deal with such cases of quacks lie with the respective state government”. The FAQ now issued by the ministry stated that there is a huge skew in the distribution of doctors between urban and rural areas with the urban to rural doctor ratio being 3.8:1.
“Consequently, most of our rural and poor population is denied good quality care leaving them in the clutches of quacks,” it added, going on to cite the figure of 57.3% of practitioners not having any medical qualification.
Quality of care of patients
Doctor-Patient ratio: 2007-14
The Times of India, September 24, 2015
Number of migrant healthcare professionals in OECD nations sees 60% rise
India continues to retain its position as the world's top supplier of expatriate doctors to 34 member countries of the Organisation for Economic Cooperation and Development (OECD), followed by China. Most new immigrants to OECD countries--taking migration statistics in totality--though, originated from China, with India occupying the fourth slot.
According to the International Migration Outlook (2015), the number of Indian expatriate doctors to the OECD jumped 55% to 86,680 in 2010-11 from 56,000 in 2000-01. The US employs 60% of the expatriate Indian doctors, with the UK being the second leading employer. China, with 26,583 expatriate doctors in 2010-11, was a distant second overall. The OECD includes, among others, the US, EU countries, Switzerland and Australia.
Philippines provided the most nurses--around 2.21 lakh--compared to India at 70,471. The number of expat nurses from India, though, has grown over the past ten years, which has seen India move to the second spot in 2010-11 from its sixth position earlier. Expat nurses from India are found primarily in the US (42%), the UK (28%) and Australia (9%).
In total, the number of migrant doctors and nurses working in OECD countries has risen 60% over the past ten years. Expat doctors and nurses constituted 23% and 14% of healthcare profes sionals in OECD countries.
“The trend mirrors the general increase in immigration to OECD countries, particularly of skilled workers,“ states the report, pointing out that a number of OECD countries have revised their migration laws in the past few years, hinging towards restriction.
Several countries have cast a greater onus on the potential employer to ensure expats only with right skills are granted employment--advertising for local employees and payment of a threshold salary for expat employees (to ensure that lower salaries don't become the sole ground for hiring expats) are among the measures adopted by various countries, especially those in EU.
The total foreign-born population in OECD countries stood at 11.7 crore people in 2013--3.5 crore more than in 2000. 2014 data suggests permanent migration flow to OECD countries reached 4.3 lakh--a 6% increase compared to 2013.
Most new immigrants to OECD countries originated from China, accounting for around 10% of migrants in 2013, followed by Romania and Poland. This is largely attributed to intra-EU mobility.Comparatively, India appeared in fourth position, with 4.4% of immigrants.
OECD countries have also seen an increase in the number of foreign students. In 2012, there were nearly 34 lakh foreign students in OECD countries--a slight rise of 3% compared to 2011. Most students in the area of higher education originated from Asia, with India accounting for 6%. International students account for an average of 8% of the OECD tertiarylevel student population.
On average see patients for 2 minutes/ 2017
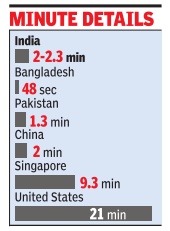
From: Malathy Iyer, Docs in India see patients for barely 2 min: Study, November 9, 2017: The Times of India
The average time that India's neighbourhood doctors, called primary care consultants, spend with patients is a negligible two minutes. Neighbouring Bangladesh and Pakistan seem worse off, with the length of medical consultation averaging 48 seconds and 1.3 minutes, respectively, according to the largest international study on consulting time, published in medical journal BMJ Open.
Contrast this with firstworld countries such as Sweden, the US or Norway where a consultation crosses 20 minutes on an average. “It is concerning that 18 countries covering around 50% of the world's population have a latest-reported mean consultation length of five minutes or less. Such a short consultation length is likely to adversely affect patient care and the workload and stress of the consulting physician,“ said the BMJ Open study conducted by researchers from various UK hospitals. Patients are the losers here, spending more at pharmacies, overusing antibiotics and sharing a poor relationship with their doctors, said the study .
The shorter consulting time could mean larger problems in the healthcare system. In the Indian context, local experts said it is a reflection of overcrowded healthcare hubs and a shortage of primary care physicians.
Primary care doctors are different from consultants trained in a particular branch of medicine.
The finding of an average two-minute consult across India didn't surprise many .Health commentator Ravi Duggal said, “It is well known that patients get less time with doctors due to overcrowding in hospitals.“ Doctors in public hospitals end up consulting two to three patients at one time due to the crowds at OPDs. “It is, hence, not uncommon for doctors to mix up symptoms between two patients,“ he said.
Private clinics and hospitals are not less crowded. “Private doctors, especially general physicians, have such crowded OPDs that they only listen to symptoms and rarely conduct a physical examination,“ said Duggal, adding that a patient's quality of care gets compromised in the process.
Former Maharashtra Medical Council member Suhas Pingle blamed overcrowded clinics and the overburdened healthcare system.
There is also India's peculiar “prescription“ of a good doctor. “In India, we believe the best doctor is one who doesn't charge and is available 24x7.This is not practical,“ said Dr Pingle. Many doctors take lower charges so that they can get more patients. “Consultation length will obviously be shorter because there are only so many hours that a doctor can work,“ said the general physician.
The main difference between western and Indian consultation is the nature of the disease. The BMJ Open study looked at the overall picture of poor primary healthcare in countries.
Rural postings
Maharashtra’s incentives, punishments/ 2015-19
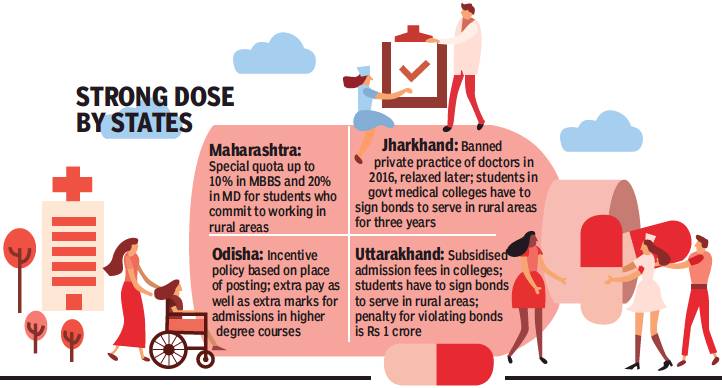
From: (With reports from Chaitanya Deshpande, Ashok Pradhan, Dhritiman Ray, Sheezan Nezami, and Shivani Azad), What gets docs to villages: Double pay, cheaper edu, salary cut, fines..., March 16, 2019: The Times of India
Maharashtra drafted a bill to create a special reservation quota up to 10% in undergraduate (MBBS) and 20% in post-graduate (MD) medical seats for those who give a commitment to work in tribal and rural areas. Candidates must serve for a period of seven years immediately after completion of MBBS and for five years after MD.
Across rural India, particularly in tribal and remote areas, the crisis in the healthcare sector has been compounded by a severe lack of doctors. States have been promoting various incentives to make new doctors opt for rural postings, but with mixed success.
“The healthcare situation in rural Maharashtra is dire. There is a huge network of 1,816 primary health centres, 400 rural hospitals, 76 sub-district hospitals and 26 civil hospitals. But this is rendered useless because of lack of manpower,” said healthcare activist Dr Amol Annadate.
The situation is perhaps worse in Odisha, which has a large population in remote areas. Now, though, it has introduced a system which is beginning to make a difference. Starting April 2015, a place of posting-based incentive policy for doctors was started by dividing the 1,750 government hospitals into five categories: from V0, the least vulnerable hospitals, to V4 the most difficult ones. These categories are based on backwardness of the area, Left-wing extremism, road/train communication, social infrastructure and distance from the capital.
Those posted in V4 category get 100% extra pay, while general medical officers in V4 hospitals get Rs 40,000 per month more and specialists Rs 80,000 additionally. There are 100 V4 and 137 V3 hospitals. Doctors working in V1 to V4 institutions get additional marks in postg raduate entrance examinations. “Young doctors are interested in joining remote and inaccessible areas to get additional marks for selection in PG courses,” health secretary Pramod Meherda said.
A doctor who has served in V4 institutions gets 10% extra marks in NEET for every year he has served, up to three years. Those who have served in V1 institutions will get 2.5% extra; V2 5% and V3 7.5%.
These measures have begun having some impact: as of December 2018, the KBK (Kalahandi-Balangir-Koraput) region had 1,072 doctors compared to 786 in March 2014.
Next door in Jharkhand, 65% of women are anemic. Vector-borne diseases like malaria, kala azar and Japanese encephalitis are endemic. Malnutrition is also above the national average. And the number of vacancies for doctors is more than half the total number of posts.
The government in 2017 began constructing three new medical colleges in Palamu, Dumka and Hazaribagh to increase the number of MBBS seats, which stands at 350 (combining medical colleges in Ranchi, Jamshedpur and Dhanbad). Three more colleges were announced in Bokaro, Koderma and Chaibasa. With existing medical colleges reeling under shortage of faculty, the retirement age of serving faculty members was raised to 65 years.
“We have a sanctioned strength of nearly 11,000 doctors in state health service, of which approximately 6,000 are vacant,” a senior official in health department said. “Doctors do not want to work in district hospitals and CHCs because the pay is low and these places are remote and have law and order problems,” the official added. Of Jharkhand’s 24 districts, 19 are affected by Maoism. That in turn has hit healthcare.
Private players were roped in to set up clinical and radiological test centres in district hospitals. In February this year, a Hyderabad based health-chain was given the nod to set up telemedicine centers in 110 CHCs. A pilot project was started in Ranchi in January whereby privately-employed doctors would be paid to visit rural health centres to set up camps and perform surgeries.
State health secretary Nitin Madan Kulkarni said, “We have rolled out a recruitment process for specialist doctors. In-principle approval has been given for additional allowances and incentives to medical officers in 2019-20.”
The Uttarakhand government has tried various carrot and stick methods to get physicians to work in remote areas.
Since 2008, MBBS courses are being offered at subsidised rates in state-run medical colleges to students who sign a bond that mandates them to serve in the hills after graduation. The subsidised fee ranges between Rs 15,000 and Rs 40,000 per year (a similar MBBS course in a private college would cost Rs 5 to Rs 7 lakh per year). However, most MBBS graduates do not honour terms of the bond even though the state government raised the penalty amount for defaulters to Rs 1 crore in 2017.
The medical education department recently issued legal notices for recovery of money to 383 doctors for not keeping their commitment to serve at least five years in the hills in exchange for subsidised education. In 2016, the health department published notices in leading dailies about those doctors who were shifted to the hills months ago but did not join duty. This was done to “name and shame” them.
Doctors, however, said lack of adequate infrastructure was the reason for their reluctance to serve in remote areas. “Even if we go to hill postings, our hands are tied because equipment available to us is not adequate. Also, emergency and trauma facilities are missing,” said Dr NS Napchyal, former general secretary of Uttarakhand Provincial Medical Health Services.
Violence
40% of govt docs face violence
Study: 40% of govt docs face violence, Mar 21, 2017: The Times of India
Nearly one in every two doctors (41%) suffers violence at public hospitals, a survey conducted at Delhi's Maulana Azad Medical College revealed. The study covered 169 junior residents and senior residents, most of them working at Lok Nayak and G B Pant hospitals, reports Durgesh Nandan Jha. Verbal abuse was the most rampant form of violence, reported by 75% of respondents who said they had suffered some form of violence. More than half of such respondents (51%) reported getting threats and 12% said they had been physically assaulted. All doctors who faced physical violence said they felt angry, frustrated and fearful.
1 in 3 healthcare staff at AIIMS faces violence
DurgeshNandan Jha, June 14, 2019: The Times of India

From: DurgeshNandan Jha , June 14, 2019: The Times of India
1 in 3 healthcare staff at AIIMS faces violence
New Delhi:
A recent study has shown that even All India Institutes of Medical Sciences (AIIMS) has not been spared from assaults against healthcare workers by irate patients and their family members. The researchers who conducted a questionnaire-based survey to assess the incidents and their impact found that one out of three healthcare workers faced violence, physical and non-physical.
While it is commonly believed that doctors face most such attacks, the study shows that nurses were the most affected by the problem, followed closely by Group-C staff and doctors.
The study published in Medical Journal Armed Forces India (MJAFI) mentions that 32 incidents of violence took place at the premier hospital in 2013 and 2014. Doctors, however, said that the reporting rate of similar incidents that occurred later remains significantly low.
“Out of 394 respondents, 136 (35%) said they had experienced workplace violence in the past 12 months and 50 (13%) physical violence,” said Dr Ruchi Garg, who conducted the study under the guidance of Dr Shakti Gupta and Dr DK Sharma over a period of 10 months from May 2014 to August 2015.
Garg said few doctors or nurses come forward to report the cases. The study concluded that the prevalence of violence against healthcare workers is quite high, but the reporting rate is significantly low due to lack of awareness. “Low reporting also creates a false sense of security in the hospital authorities, and they often fail to initiate necessary remedial measures to curb it,” it added.
Dr Gupta, the medical superintendent of AIIMS’ RP Eye Centre, said most incidents of violence occur due to a communication gap. “Our staff is overworked due to heavy patient rush. Sometimes, there is a gap in communicating or delay in attending to the needs of patients. This leads to altercations. The incidence rate has come down significantly in the last few years,” he added.
“AIIMS has a grievance redressal committee in every centre to address such issues so that the matter doesn’t get out of hand. Similar steps should be taken by other hospitals, in addition to improving the infrastructure and imparting soft skills to healthcare workers,” Dr Gupta said.
Dr Vijay Gurjar, former president of AIIMS’ Resident Doctors’ Association (RDA), said there were some incidents of violence against the hospital staff in 2017 and 2018 too. “We held protests to seek action against the perpetrators. We also started a helmet protest to flag our concerns as well as self-defence classes for doctors,” he added.
State-wise
Mumbai: 2016-21
Swati Deshpande, May 28, 2021: The Times of India
The state government told Bombay high court that since 2016 till April 2021, there were 674 cases of violence against doctors registered and a committee was set up on March 24 to review the 2010 Maharashtra Medicare Act meant to protect doctors and hospitals against violence.
The committee is set to meet for a final meeting by May- end and any amendment to the act considered necessary to make it effective would be decided after “following due legal procedure.’’ The state said also to ensure greater security, police have been asked to do beat patrolling around hospitals too to check with police guards there.
The state’s reply was in a PIL filed by Dr Rajeev Joshi from Pune before a vacation bench of Justices Amjad Sayed and Girish Kulkarni.
Advocate Nitin Deshpande appearing for Dr Joshi said the state’s fresh affidavit of Thursday did not appear detailed enough. The HC asked that it be served on advocates Rui Rodrigues and Sudeep Nargolkar for interveners the Association of Medical Consultants and Association for Hospitals in Pune too, while adjourning it to June for further hearing.
"Women doctors": the term
In brief
July 18, 2021: The Times of India
Did you choose to title the book ‘Lady Doctors’ ironically?
It’s unironical because that is what these women were called back then, when women doctors were an anomaly. The earliest mention I could find of this term was in the British Medical Journal in 1870, when lady doctors were called “a traitress to their sex.”
In cloistered, colonial India, what kind of labels did these women attract for their decision to pursue medicine?
Kadamabini Ganguly was called a whore, Rukhmabai was called dissolute, and compared to an adulteress, a thief and killer. Haimabati Sen got death threats when she won a gold medal. Mary Poonen Lukose was criticised for her foreign education, and told that she needed to cultivate ‘Indian manners’.
Of the six Indian ‘lady doctors’ of 19th-century India that your book focuses on, whose story made the most impact on you?
Probably Rukhmabai Raut because she walked away from a child marriage, spent years in court to divorce her husband, defied powerful conservatives, went to the UK to study, and eventually led a long and fulfilling life as a doctor in Rajkot and Surat. Even one of these would be a huge achievement. Combined, it is almost unbelievable.
Were the men in their lives supportive?
Nearly all the women were supported by their fathers to study. The husbands were sometimes allies, sometimes hindrances. Anandibai’s husband encouraged her to study but was also physically abusive. Haimabati’s husband did not object to her being a doctor but took all her earnings and occasionally hit her. On the other hand, Kadambini and Mary Poonen Lukose’s husbands are widely reported to have been supportive. In fact, most of the misogyny they faced was from their mothers and female relatives who discouraged their studies.
Despite their foreign education, the women doctors had to earn the trust of patients in India. What lengths did they go to?
Kadambini had to go to the UK to get a British education, because people were reluctant to trust a doctor with an Indian education. Rukhmabai grabbed a pregnant sheep and delivered its lamb in her hospital to convince women to come for their deliveries. Mary Poonen Lukose only gained the trust of the community after she delivered the Travancore Rani’s babies.
Many of these women doctors had to work in the backdrop of famine and disease. What can they teach us about living with Covid-19?
I think Mary Poonen Lukose’s comments on smallpox vaccination are very revealing of how Covid will eventually have to be overcome, with immense sacrifice from the public. In 1925, Mary opposed a resolution in the Travancore Legislative Assembly, which sought to make smallpox vaccinations optional. She said, “Petty inconveniences and even risks have to be encountered by individuals for the sake of the greater good of the community as a whole.”
While reading their diaries and memoirs, what were the things that struck you?
The thing that struck me instantly was how advanced their views were. Even Anandibai, who outwardly played the part of the good Indian wife, displayed absolutely no fear about crossing the seas alone, at a time when women were completely dependent on their husbands. Indeed, she said, “If this life is so transitory, why depend on another?”
Did their sense of humour surprise you?
Haimabati’s sarcasm about her useless husband definitely surprised me. Particularly that line in her memoir, “My husband came home and immediately began to ride his high horse. He said, ‘Women are but thorns on the way of life, hindrances to spiritual quest”. An elderly lady told him off, “If you have decided to spend your life in spiritual pursuits, why did you marry?”
Would the six women doctors have laughed at the term ‘work-life balance’?
Probably yes! Most of them accepted that they would be both working and raising families with very little help. But just because they did not know about the term, doesn’t mean it was easy. A frustrated Muthulakshmi, for instance, once wrote that women doctors were better off staying unmarried because of the tough balancing act.
Would you call all six of them feminists?
Certainly, they were all feminists because they all believed that women were as capable as men of being doctors. Before the concept of equal pay for equal work became accepted in India, Haimabati Sen wrote angrily about how she was paid less for her work than men. Rukhmabai wrote at length about how marriage was an institution that benefited only men, not women. I would describe their brand of feminism, overall, as radical for their time. Or indeed even for our times!
See also
Doctors in India
Medical education and research: India
Medical malpractice, negligence: India
Institute of Post Graduate Medical Education and Research, Kolkata
Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER), Puducherry